Antibiotics represent a cornerstone of modern medicine, combating bacterial infections and significantly reducing morbidity and mortality rates. Understanding the sources from which these life-saving drugs are derived is crucial for appreciating their development and potential limitations.
The Origins of Antibiotics
Antibiotics are not a homogenous group; they originate from diverse sources, reflecting the ingenuity of scientific discovery and the remarkable capabilities of microorganisms. These sources can be broadly categorized as follows:
1. Natural Sources: Microorganisms
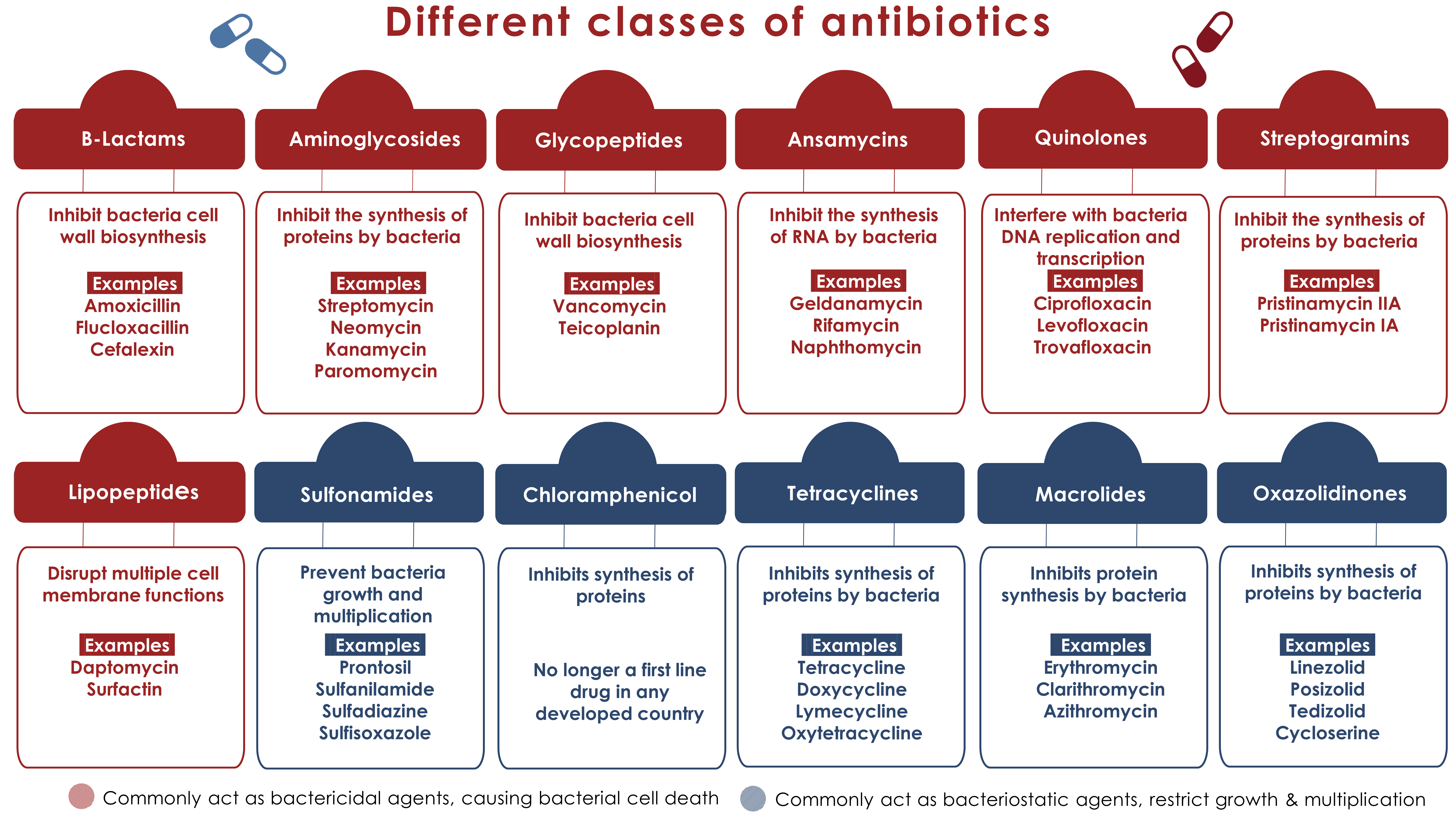
The vast majority of antibiotics are derived from naturally occurring compounds produced by microorganisms, primarily bacteria and fungi. These organisms synthesize these substances as a defense mechanism, inhibiting the growth or killing competing microorganisms in their environment. This interspecies competition is a major driver of antibiotic production.
"The discovery of penicillin by Alexander Fleming in 1928 marked a turning point in medicine, revealing the potential of microorganisms to produce potent antibacterial agents."
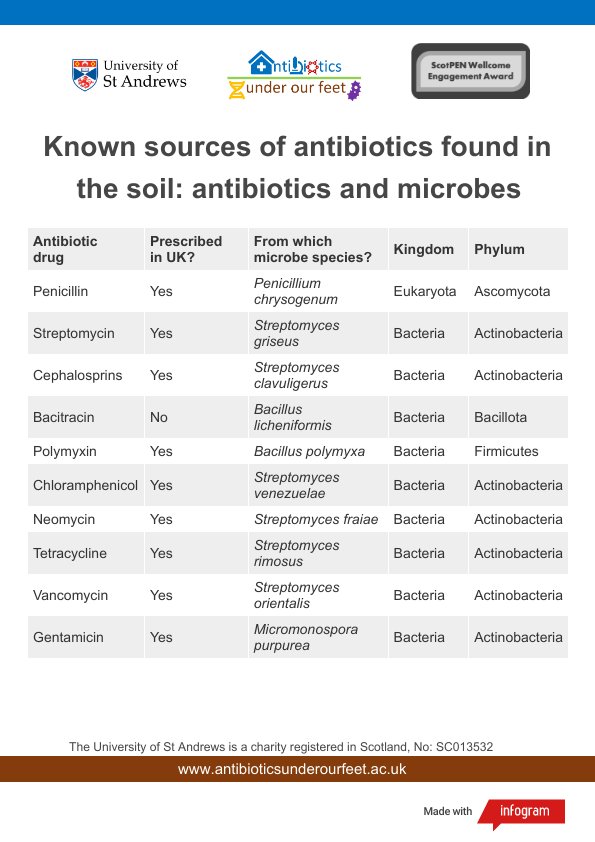
Examples of antibiotics derived from microorganisms include:
- Penicillin: Famously discovered from the Penicillium notatum fungus.
- Streptomycin: Isolated from the bacterium Streptomyces griseus.
- Tetracycline: Produced by Streptomyces species.
- Erythromycin: Derived from Saccharopolyspora erythraea.
- Vancomycin: Isolated from Amycolatopsis orientalis.
These microorganisms are typically found in soil, where they engage in complex ecological interactions. Scientists screen soil samples for microorganisms that exhibit antibacterial activity, subsequently isolating and identifying the active compounds.
2. Semi-Synthetic Sources: Chemical Modification of Natural Compounds
While many antibiotics are directly derived from natural sources, others are created through chemical modification of these natural compounds. This process is known as semi-synthesis and allows scientists to enhance the properties of existing antibiotics, such as:
- Increased potency: Making the antibiotic more effective against bacteria.
- Improved bioavailability: Enhancing the absorption and distribution of the drug in the body.
- Broader spectrum of activity: Expanding the range of bacteria that the antibiotic can target.
- Reduced side effects: Minimizing adverse reactions in patients.
- Increased resistance to bacterial degradation: Making the antibiotic less susceptible to inactivation by bacterial enzymes.
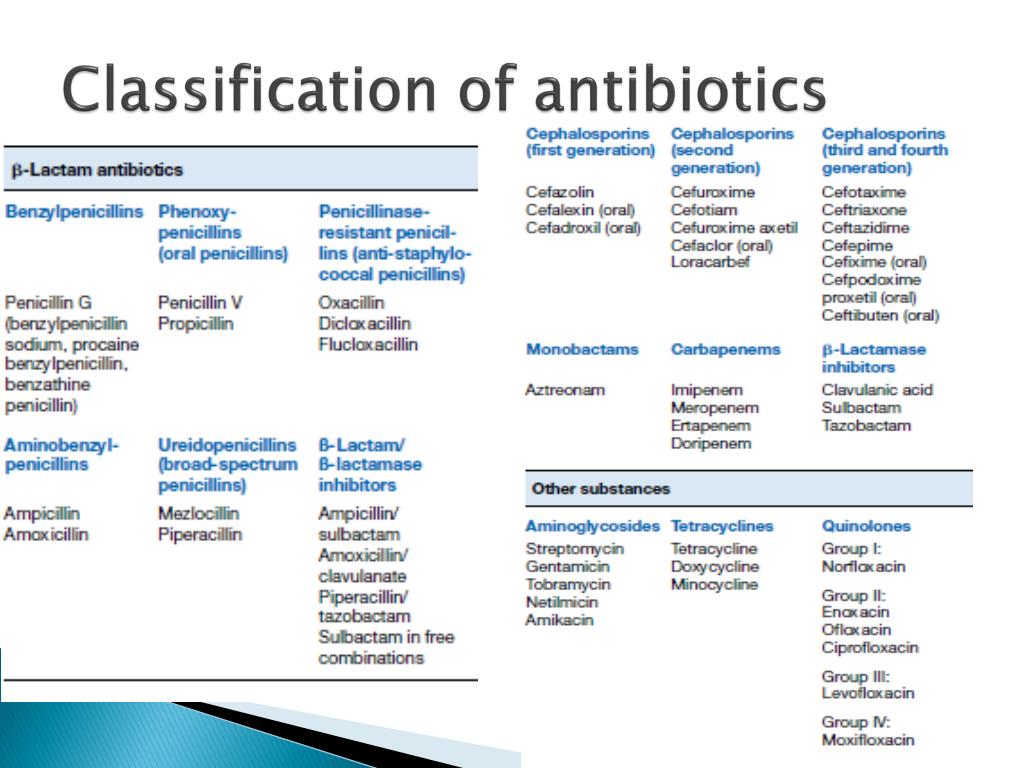
Examples of semi-synthetic antibiotics include:
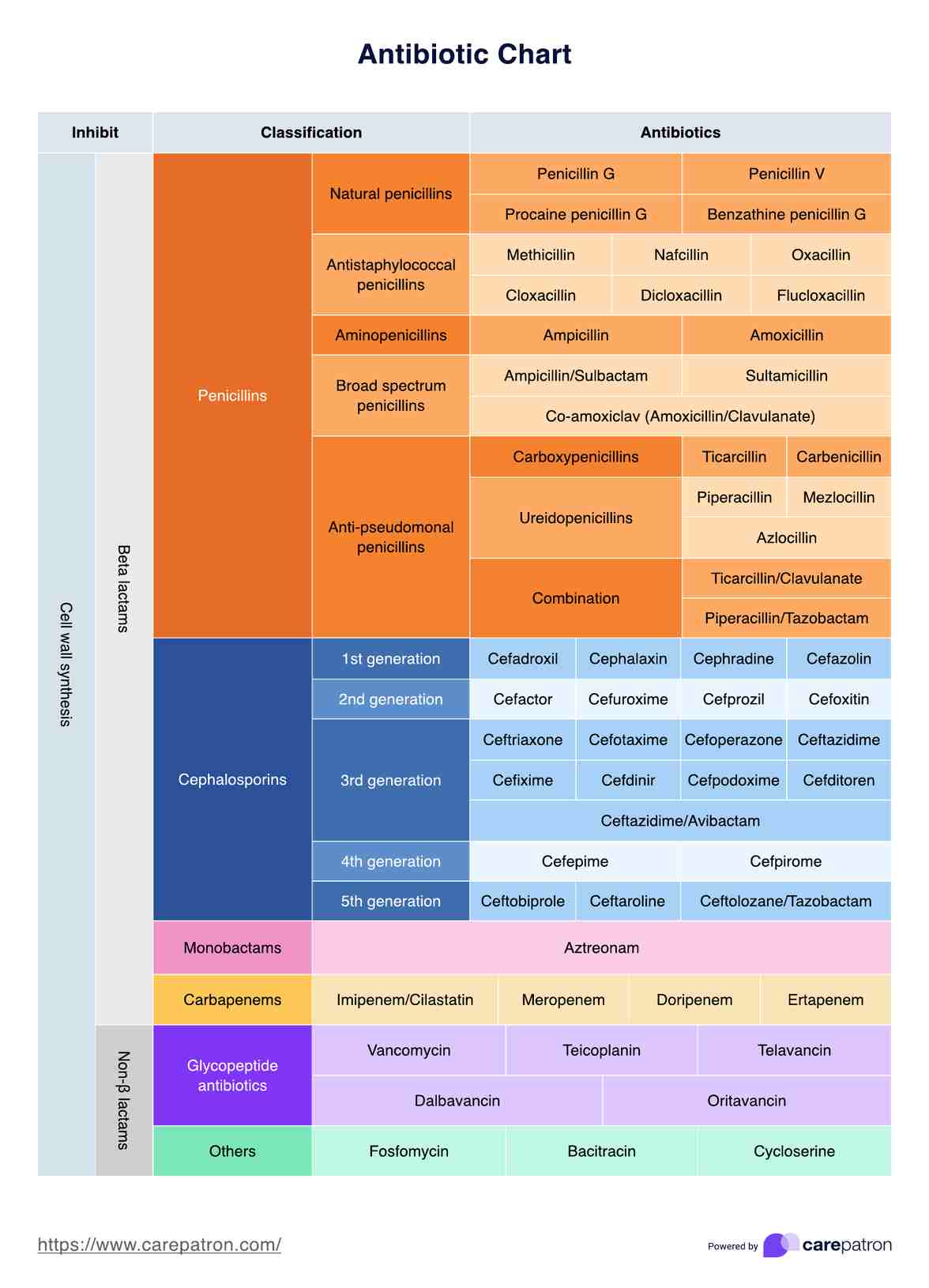
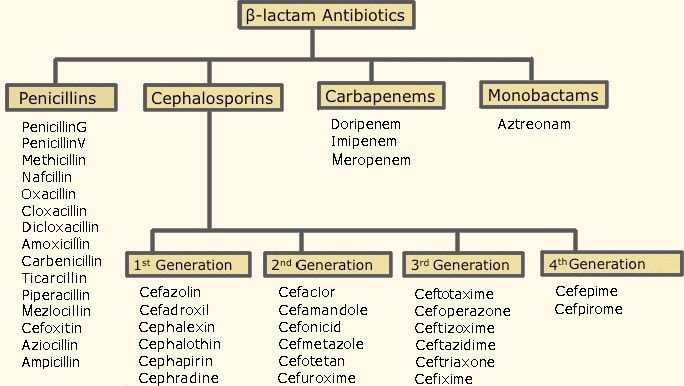
- Methicillin: A semi-synthetic penicillin derivative.
- Ampicillin: Another semi-synthetic penicillin derivative with a broader spectrum than penicillin.
- Cephalosporins: A large class of antibiotics derived from cephalosporin C, produced by the fungus Acremonium chrysogenum, and subsequently modified chemically.
Semi-synthesis involves taking a naturally produced antibiotic as a starting point and then chemically altering its structure to optimize its pharmacological properties. This approach allows for the creation of novel antibiotics with improved characteristics, addressing limitations of naturally occurring compounds.
3. Synthetic Sources: Chemical Synthesis in the Laboratory
Some antibiotics are entirely synthesized in the laboratory through chemical reactions. These synthetic antibiotics are not based on naturally occurring compounds, but rather are designed and created from scratch. This approach offers the greatest flexibility in terms of designing antibiotics with specific properties.
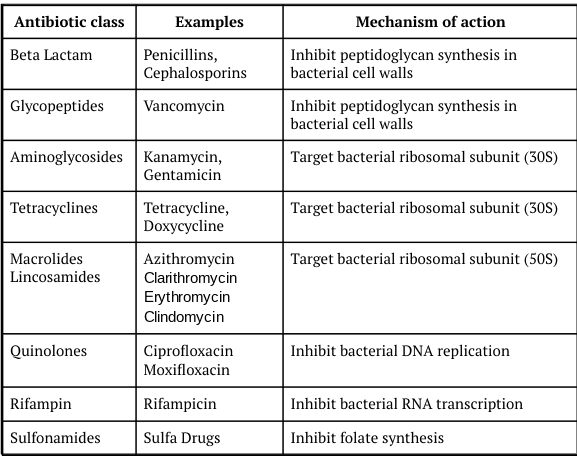
Examples of synthetic antibiotics include:
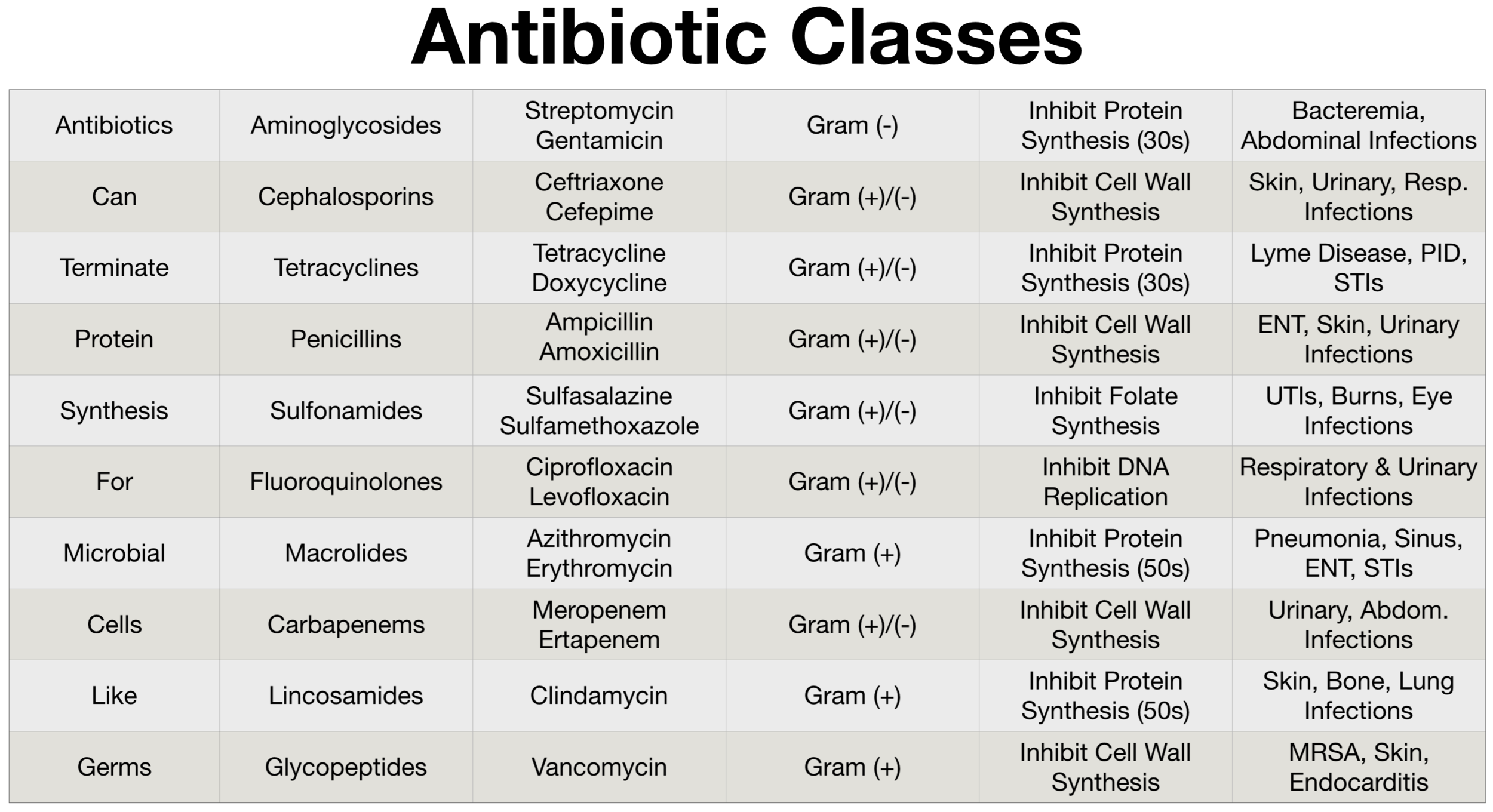
- Quinolones (e.g., ciprofloxacin, levofloxacin): These antibiotics inhibit bacterial DNA replication.
- Oxazolidinones (e.g., linezolid): These antibiotics inhibit bacterial protein synthesis.
- Sulfonamides (e.g., sulfamethoxazole): These antibiotics inhibit bacterial folate synthesis.
The development of synthetic antibiotics often involves a process of drug discovery, where scientists screen large libraries of chemical compounds for antibacterial activity. This process can be time-consuming and expensive, but it can lead to the discovery of novel antibiotics that are effective against resistant bacteria.
Identifying Incorrect Sources: What Antibiotics Are NOT Derived From
Given the diverse origins of antibiotics, it is equally important to understand what they are not derived from. Misconceptions about antibiotic sources can lead to misunderstandings about their function and limitations.
Antibiotics are NOT derived from the following:
- Viruses: Antibiotics target bacteria, not viruses. Viruses are treated with antiviral medications.
- Human cells: Antibiotics are not produced by or derived from human cells or tissues.
- Animal cells (directly): While some animal products may have antimicrobial properties, antibiotics themselves are not directly derived from animal cells in the same way they are from bacteria or fungi.
- Minerals (directly): While certain minerals like silver have antimicrobial properties, antibiotics as pharmaceutical drugs are not directly mined or extracted from minerals.
- Simple organic compounds (directly): While antibiotics are organic compounds, they are complex molecules synthesized by microorganisms or created through complex chemical processes, not directly derived from simple organic building blocks like sugars or amino acids without significant modification.
The key distinction lies in the complexity of the antibiotic molecule and the process of its creation. Naturally derived antibiotics are complex molecules synthesized by living organisms. Semi-synthetic antibiotics are modifications of these naturally occurring molecules. Synthetic antibiotics are complex molecules designed and synthesized through complex chemical processes.
Practical Advice and Insights
Understanding the sources of antibiotics can inform our approach to their use and the challenge of antibiotic resistance:
- Responsible antibiotic use: Recognize that antibiotics are powerful drugs with specific targets. Using them inappropriately (e.g., for viral infections) contributes to antibiotic resistance.
- Source awareness: Knowing that most antibiotics originate from microorganisms highlights the importance of preserving biodiversity, particularly in soil ecosystems, which are reservoirs of antibiotic-producing organisms.
- Support research and development: The development of new antibiotics is a complex and expensive process. Supporting research efforts is crucial for addressing the growing threat of antibiotic resistance.
- Promote hygiene: Simple hygiene practices, such as handwashing, can prevent the spread of bacterial infections and reduce the need for antibiotics.
- Vaccination: Vaccinations can prevent many bacterial infections, reducing the reliance on antibiotics.
By understanding the origins and limitations of antibiotics, we can contribute to their responsible use and help ensure their continued effectiveness in combating bacterial infections.