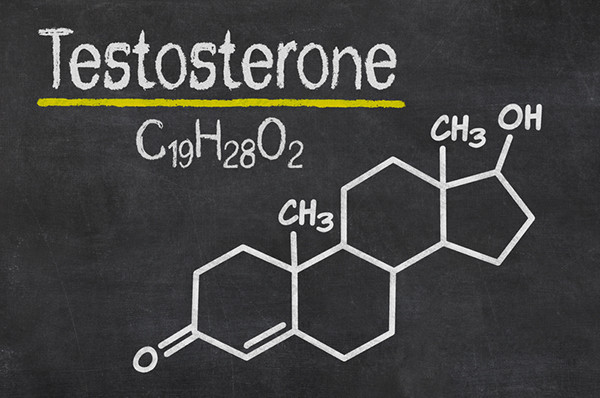
Testosterone, often hailed as the primary male sex hormone, plays a critical role in various physiological functions within the human body, impacting everything from muscle mass and bone density to mood and libido. While often discussed as a single entity, testosterone actually exists in different forms within the bloodstream. Understanding these distinctions is crucial for comprehending how testosterone affects the body and how hormonal imbalances are diagnosed and treated.
The Forms of Testosterone in the Body
Testosterone circulates in the bloodstream in three primary forms:
- Bound to Sex Hormone-Binding Globulin (SHBG): This is the most prevalent form. SHBG is a protein produced by the liver that binds tightly to testosterone, rendering it biologically inactive. Because of this strong bond, testosterone attached to SHBG cannot easily interact with cells to exert its effects.
- Bound to Albumin: Albumin is another protein in the blood that binds to testosterone, though with a weaker affinity than SHBG. Testosterone bound to albumin is considered loosely bound, and it can dissociate from albumin more readily, making it potentially available for use by tissues.
- Free Testosterone: This is the unbound form of testosterone that is not attached to any protein. It represents only a small fraction of the total testosterone in the bloodstream, but it is the biologically active form that can directly interact with cells and exert its effects.
Total Testosterone vs. Bioavailable Testosterone
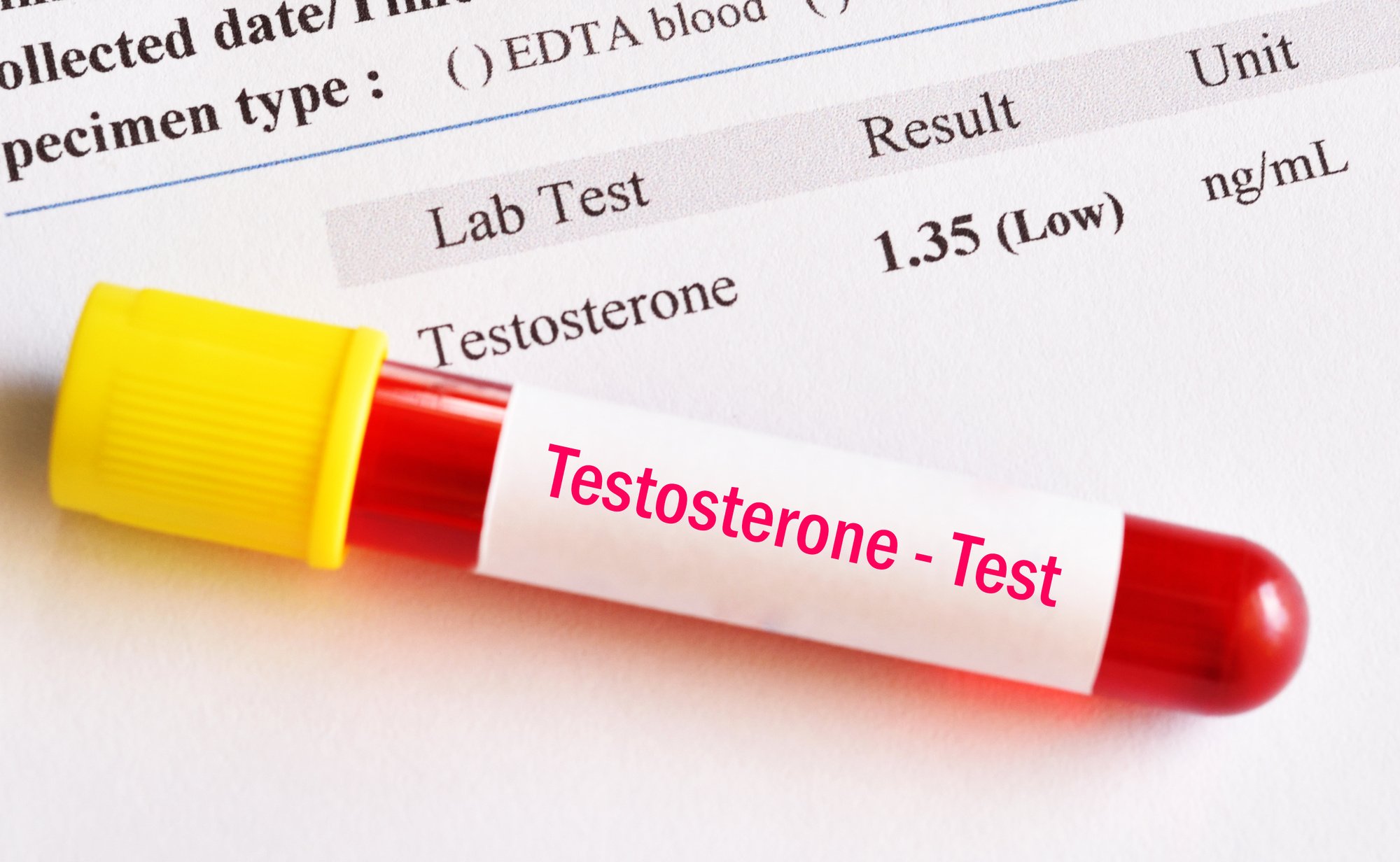
When doctors order a testosterone test, they often measure total testosterone, which represents the sum of all three forms: SHBG-bound, albumin-bound, and free testosterone. While total testosterone provides a general overview, it doesn't always paint a complete picture of hormonal activity. This is because SHBG levels can vary significantly from person to person, influencing the proportion of testosterone that is biologically available.
Bioavailable testosterone is the sum of free testosterone and albumin-bound testosterone. This measurement is often considered a more accurate reflection of the amount of testosterone that is available for the body to use. In some cases, particularly when SHBG levels are abnormal, measuring bioavailable testosterone can provide a more clinically relevant assessment of testosterone status than total testosterone alone.
The Importance of Free Testosterone
As mentioned above, free testosterone is the biologically active form that directly interacts with cells. It enters cells and binds to androgen receptors, triggering a cascade of events that influence gene expression and protein synthesis. This, in turn, impacts a wide range of physiological processes, including:
- Muscle Growth and Strength: Testosterone promotes muscle protein synthesis, leading to increased muscle mass and strength.
- Bone Density: Testosterone plays a crucial role in maintaining bone density, protecting against osteoporosis.
- Libido and Sexual Function: Testosterone is essential for sexual desire, erectile function, and sperm production.
- Mood and Cognitive Function: Testosterone influences mood, energy levels, and cognitive performance, including memory and concentration.
- Red Blood Cell Production: Testosterone stimulates the production of red blood cells, which carry oxygen throughout the body.
Given its direct impact on these vital functions, the level of free testosterone is often considered a more sensitive indicator of testosterone deficiency than total testosterone alone. For example, an individual with normal total testosterone but high SHBG may have a low level of free testosterone, leading to symptoms of hypogonadism (testosterone deficiency).
Factors Influencing Testosterone Levels and SHBG
Several factors can influence both total and free testosterone levels, as well as the concentration of SHBG in the blood:
- Age: Testosterone levels naturally decline with age, typically starting in the late 30s or early 40s. This age-related decline can lead to a decrease in both total and free testosterone.
- Obesity: Excess body fat, particularly visceral fat (fat around the abdominal organs), can lower testosterone levels. Adipose tissue contains an enzyme called aromatase, which converts testosterone into estrogen.
- Medical Conditions: Certain medical conditions, such as type 2 diabetes, chronic kidney disease, and liver disease, can affect testosterone production and SHBG levels.
- Medications: Some medications, including opioids, corticosteroids, and certain antidepressants, can interfere with testosterone production or increase SHBG levels.
- Lifestyle Factors: Chronic stress, poor sleep, and lack of physical activity can negatively impact testosterone levels.
- Genetics: Genetic factors can also influence testosterone levels and SHBG production.
Clinical Significance of Understanding Testosterone Forms
Understanding the different forms of testosterone is crucial for accurate diagnosis and effective treatment of testosterone deficiency. When evaluating a patient for possible hypogonadism, healthcare providers should consider not only total testosterone but also SHBG and, if necessary, free or bioavailable testosterone. This comprehensive assessment helps to determine the true extent of testosterone deficiency and to tailor treatment accordingly.
For instance, if a patient presents with symptoms of low testosterone (e.g., fatigue, decreased libido, muscle loss) but has a normal total testosterone level, further investigation of SHBG and free testosterone is warranted. If SHBG is elevated and free testosterone is low, the patient may still benefit from testosterone therapy, even though the total testosterone level is within the normal range. Conversely, if a patient has low total testosterone but normal SHBG and free testosterone, the symptoms may be due to other underlying conditions.
Furthermore, monitoring the response to testosterone therapy often involves tracking both total and free testosterone levels to ensure that the patient is receiving an adequate dose and that the therapy is effectively restoring biologically active testosterone to optimal levels.
"In conclusion, while often discussed as a single entity, testosterone exists in different forms, each with its own role and significance. Understanding these distinctions is vital for accurate diagnosis and effective management of testosterone-related conditions."
Why This Matters
Distinguishing between the different types of testosterone – SHBG-bound, albumin-bound, and free – is crucial because only free testosterone is readily available for the body to use. Measuring total testosterone alone can be misleading, as it doesn't account for variations in SHBG levels, which can significantly impact the amount of free testosterone available. Accurately assessing free testosterone, or bioavailable testosterone, helps healthcare providers diagnose and treat testosterone deficiency more effectively, ensuring that individuals receive the appropriate care to optimize their health and well-being. This knowledge is essential for anyone concerned about hormonal health, as it emphasizes the importance of a comprehensive evaluation when assessing testosterone levels.