Fungal infections are a common ailment affecting millions worldwide. While conventional treatments such as topical and oral antifungal medications are often effective, they can sometimes present challenges due to side effects, drug resistance, or limited efficacy in certain cases. Consequently, researchers have been exploring alternative and adjunctive therapies, and one promising avenue is blue light therapy.
Understanding Fungal Infections
Fungal infections, also known as mycoses, are caused by microscopic fungi that invade and colonize various parts of the body. These infections can range from superficial skin conditions to more serious systemic illnesses.
Common Types of Fungal Infections
Several types of fungal infections are frequently encountered, including:
- Athlete's Foot (Tinea Pedis): Affects the skin of the feet, often causing itching, burning, and scaling, particularly between the toes.
- Ringworm (Tinea Corporis): Presents as circular, raised, and scaly patches on the skin. Despite its name, it's caused by a fungus, not a worm.
- Nail Fungus (Onychomycosis): Infects the nails, causing them to thicken, discolor, and become brittle.
- Yeast Infections (Candidiasis): Caused by Candida species, commonly affecting the mouth (thrush), vagina (vaginal yeast infection), or skin folds.
- Aspergillosis: An infection caused by Aspergillus, usually affecting the lungs but can spread to other organs, particularly in individuals with weakened immune systems.
The severity and treatment of fungal infections vary depending on the type of fungus, the location of the infection, and the individual's overall health.
What is Blue Light Therapy?
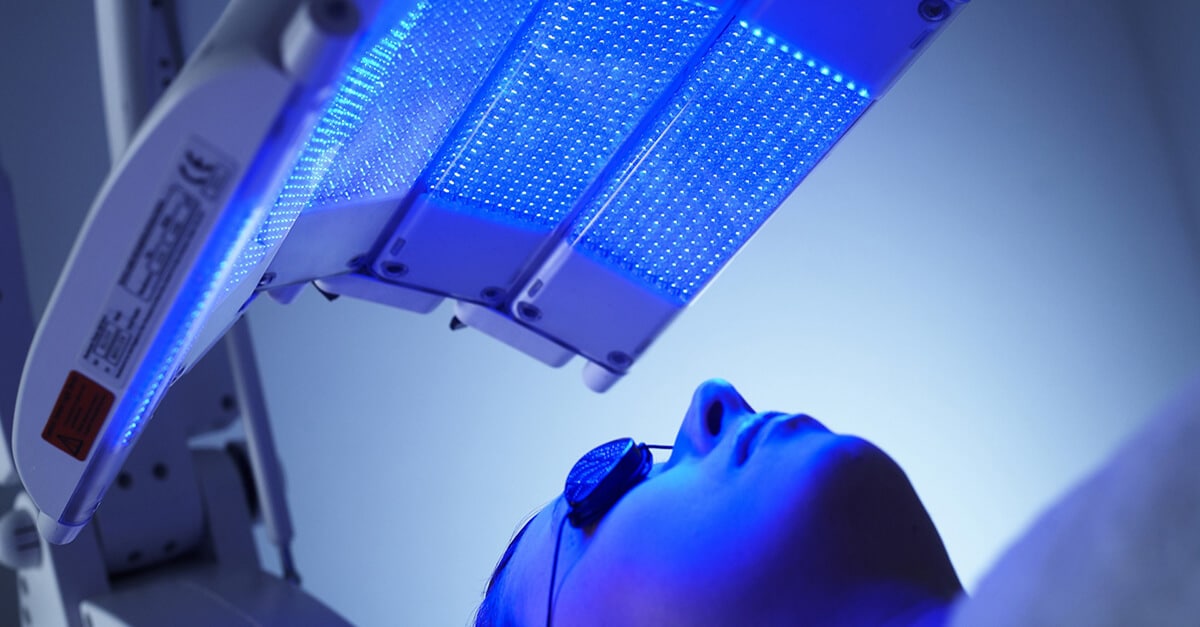
Blue light therapy, also known as phototherapy with blue light, involves exposing the affected area to a specific wavelength of blue light, typically in the range of 400-470 nanometers. This type of light is considered part of the visible light spectrum and is distinct from ultraviolet (UV) light, which is known for its damaging effects on the skin.
The therapeutic effects of blue light stem from its ability to interact with certain molecules within cells, particularly porphyrins. Porphyrins are naturally occurring compounds found in bacteria, including those associated with acne, and also in fungi. When blue light interacts with porphyrins, it triggers a photochemical reaction that generates reactive oxygen species (ROS), such as singlet oxygen. These ROS are toxic to the cells, leading to their inactivation or death.
Blue light therapy is a non-invasive treatment option. It is generally administered using LED (light-emitting diode) devices that emit a concentrated beam of blue light. The treatment sessions are typically short, lasting from a few minutes to half an hour, and may be repeated over several weeks, depending on the condition being treated.
Blue Light Therapy and Fungal Infections: The Science
The application of blue light therapy for fungal infections is based on the principle that fungi, like certain bacteria, contain porphyrins. When exposed to blue light, these porphyrins produce ROS, leading to fungal cell damage and ultimately inhibiting their growth and proliferation.
Several studies have explored the efficacy of blue light therapy against various types of fungi. In vitro studies (experiments performed in a laboratory setting) have shown that blue light can effectively kill or inhibit the growth of common fungal species, including Candida albicans (responsible for yeast infections) and dermatophytes (the fungi that cause athlete's foot, ringworm, and nail fungus). The mechanism is thought to involve the disruption of fungal cell membranes and the inactivation of essential enzymes.
In vivo studies (experiments performed on living organisms) are still limited, but some have demonstrated promising results. For example, some clinical trials have investigated the use of blue light therapy for the treatment of onychomycosis (nail fungus). These studies have shown that blue light can reduce the severity of nail infections and improve the appearance of affected nails, although the results may not be as dramatic as those achieved with conventional antifungal medications. The advantage, however, is the reduced risk of systemic side effects.
The specific wavelengths and dosages of blue light used in these studies vary, but generally, higher doses and longer treatment times are more effective. However, it's important to balance efficacy with safety to avoid any potential side effects, such as skin irritation or redness.
Advantages and Limitations
Advantages
- Non-invasive: Blue light therapy is a non-surgical and non-pharmacological approach to treating fungal infections.
- Minimal Side Effects: Compared to oral antifungal medications, blue light therapy is generally associated with fewer side effects. The most common side effect is mild skin redness or irritation, which usually resolves quickly.
- Potential for Combination Therapy: Blue light therapy can be used in conjunction with conventional antifungal treatments to enhance their efficacy. It can also be an option for patients who cannot tolerate or have contraindications to systemic antifungal medications.
- Targeted Treatment: Blue light targets the affected area directly, minimizing the exposure of other parts of the body to the treatment.
Limitations
- Limited Clinical Evidence: While promising, the clinical evidence supporting the use of blue light therapy for fungal infections is still limited, especially in in vivo studies. More large-scale, well-controlled clinical trials are needed to confirm its efficacy and determine the optimal treatment parameters.
- Variable Efficacy: The effectiveness of blue light therapy may vary depending on the type of fungal infection, the severity of the infection, and the individual's response to treatment.
- Time Commitment: Blue light therapy typically requires multiple treatment sessions over several weeks or months, which may be a deterrent for some patients.
- Cost: The cost of blue light therapy devices and treatments can be a factor for some individuals.
The Future of Blue Light Therapy for Fungal Infections
Blue light therapy represents a promising, albeit still evolving, approach to managing fungal infections. Ongoing research is focused on:
- Optimizing the wavelengths and dosages of blue light for different types of fungal infections.
- Developing more effective and user-friendly blue light therapy devices.
- Conducting larger clinical trials to evaluate the efficacy and safety of blue light therapy in diverse populations.
- Investigating the potential of combining blue light therapy with other antifungal treatments or adjunctive therapies.
As the evidence base grows, blue light therapy may become a more widely accepted and integrated treatment option for fungal infections, offering a safe and effective alternative or complement to conventional therapies.
Conclusion
Blue light therapy offers a potential alternative or adjunct treatment for fungal infections, leveraging the light's interaction with fungal porphyrins to disrupt cellular function. While research is ongoing, its non-invasive nature and minimal side effects make it an appealing option, particularly when conventional treatments are not fully effective or poorly tolerated. Further studies are needed to optimize its application and fully establish its role in combating these common infections.