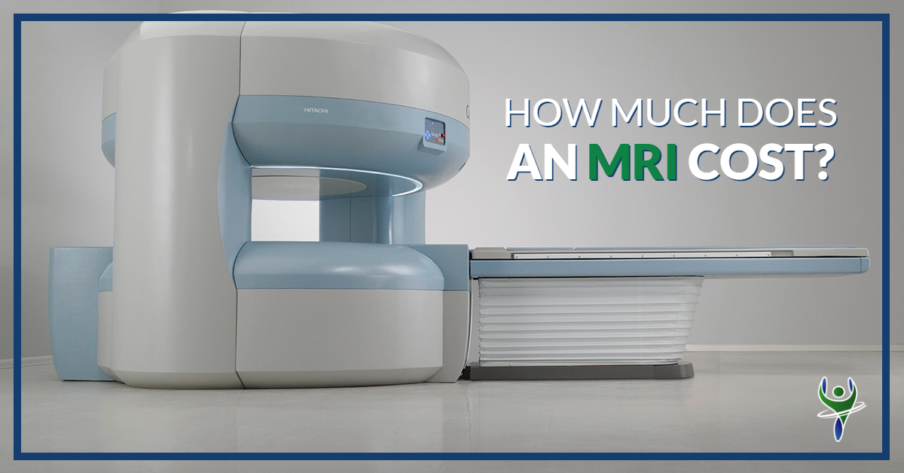
Understanding Aflac's coverage for Magnetic Resonance Imaging (MRI) procedures requires navigating the specifics of your individual policy. Aflac operates as a supplemental insurance provider, meaning its policies are designed to pay cash benefits directly to the policyholder, regardless of other existing insurance coverage. This benefit is intended to help offset out-of-pocket expenses associated with medical treatments, including MRIs.
Determining Your Aflac MRI Benefit
The amount Aflac pays for an MRI is not a fixed amount. It depends heavily on several key factors:
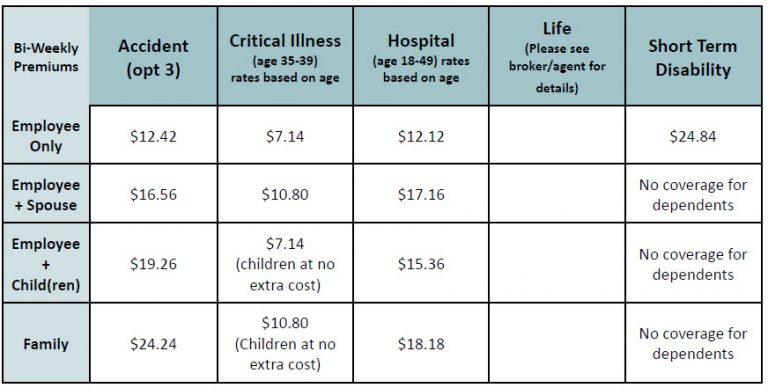
Policy Type and Coverage Levels
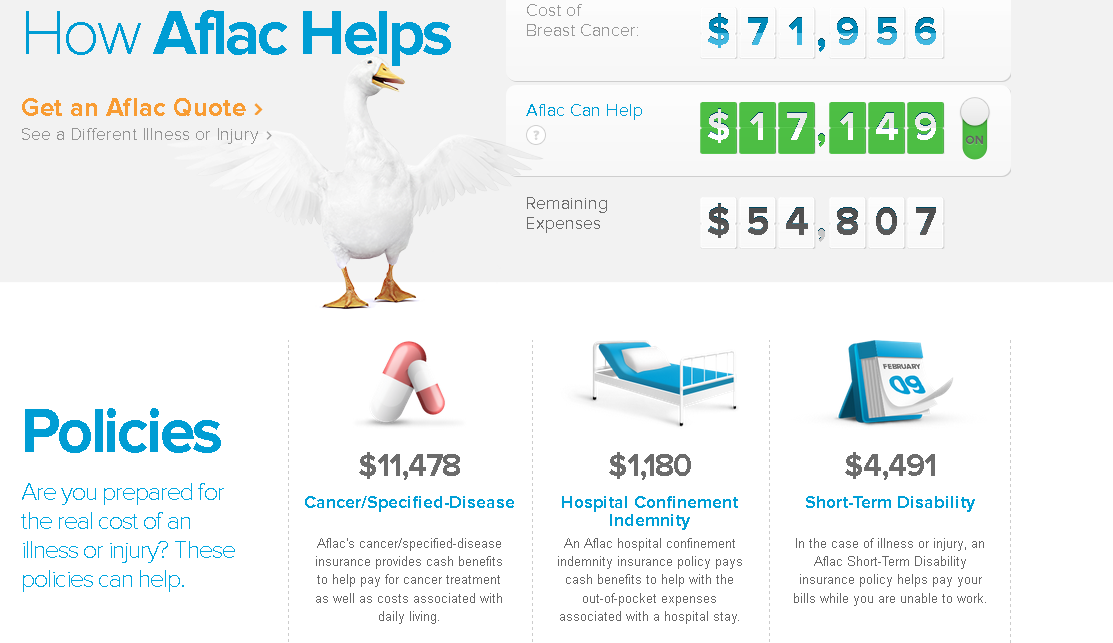
Aflac offers various policy types, such as accident, hospital indemnity, and critical illness plans. Each policy has different schedules of benefits. The benefit for diagnostic procedures like MRIs will be specifically outlined within the policy documents. Always refer to your policy certificate or speak with an Aflac representative to confirm the exact coverage details. Some policies may have a flat benefit amount for specific diagnostic tests, while others might offer coverage based on a percentage of the total cost or a daily hospital confinement benefit that can be applied.
Diagnostic Test Benefit
Many Aflac policies feature a "Diagnostic Test" benefit. This section specifically addresses coverage for procedures used to diagnose medical conditions. The wording in your policy will describe which tests are covered and the corresponding benefit amount. It's important to note that some policies may differentiate between MRIs performed in a hospital versus an outpatient setting, with potentially different benefit amounts for each.
For example, your policy might state: "Diagnostic Test Benefit: $100 for covered diagnostic tests, including X-rays, CT scans, and MRIs." In this scenario, Aflac would pay $100 towards the cost of your MRI, regardless of the total cost of the procedure.
Hospital Confinement Benefit
If your MRI requires a hospital stay, even for observation, your Aflac policy's "Hospital Confinement" benefit might be triggered. This benefit pays a daily amount for each day you are confined to a hospital. The amount varies depending on the policy. While this benefit isn't specifically for the MRI itself, it can help cover expenses incurred during your hospital stay, indirectly contributing to the overall cost of the MRI episode.
For example, if your policy states: "Hospital Confinement Benefit: $500 per day," and you are hospitalized for one day due to the MRI, you would receive $500 from Aflac.
Factors Affecting Aflac Claim Payout
Even after understanding your policy’s potential benefits, several factors can influence the actual amount you receive from Aflac:
Waiting Periods
Many Aflac policies have waiting periods, also known as elimination periods, before certain benefits become payable. This means that if you purchase a policy and undergo an MRI shortly thereafter, you may not be eligible for benefits if the waiting period has not yet elapsed. Check your policy’s effective date and any applicable waiting periods for diagnostic tests.
Pre-existing Conditions
Some Aflac policies may have limitations or exclusions related to pre-existing conditions. If the MRI is related to a condition that existed before you enrolled in the policy, Aflac might not pay benefits. Review your policy's pre-existing condition clause carefully.
Coordination of Benefits (If Applicable)
Aflac generally pays benefits regardless of other insurance you may have. However, in rare cases, there might be coordination of benefits clauses, especially if you have multiple Aflac policies covering the same event. In this scenario, Aflac may coordinate payments to avoid overpayment.
Proper Claim Submission
Submitting a complete and accurate claim is crucial for receiving prompt payment from Aflac. You will typically need to provide the following:
- A completed claim form.
- A copy of the itemized bill from the medical provider (radiology center or hospital).
- Diagnostic codes (ICD-10 codes) related to the MRI.
- Potentially, a copy of the MRI report.
Follow Aflac's claim submission instructions carefully to avoid delays or denials.
Examples of Aflac MRI Benefit Scenarios
To illustrate how Aflac might pay for an MRI, consider these scenarios:
Scenario 1: Outpatient MRI with Diagnostic Test Benefit Only
You undergo an outpatient MRI that costs $1,200. Your Aflac policy has a Diagnostic Test Benefit of $150 for MRIs. Aflac would pay you $150, regardless of your other insurance coverage or the total cost of the MRI.
Scenario 2: MRI Requiring One-Day Hospital Stay
Your MRI requires a one-day hospital stay for monitoring. The MRI itself costs $1,500, and the hospital stay costs $2,000. Your Aflac policy has a Diagnostic Test Benefit of $100 for MRIs and a Hospital Confinement Benefit of $400 per day. Aflac would pay you $100 for the MRI and $400 for the hospital stay, totaling $500.
Scenario 3: MRI Related to a Pre-Existing Condition (Exclusion)
You undergo an MRI to investigate back pain, but the MRI is related to a pre-existing spinal condition that was diagnosed before you enrolled in your Aflac policy. Your policy has a pre-existing condition exclusion for the first 12 months of coverage. Aflac would likely deny the claim because the MRI is related to a pre-existing condition within the exclusion period.
How to Find Your Specific Aflac Policy Information
The most reliable way to determine your Aflac MRI benefits is to consult your policy documents. Look for:
- Your policy certificate: This document outlines the specific benefits and coverage levels you have purchased.
- The schedule of benefits: This section details the amounts Aflac will pay for various medical procedures and events.
- The definitions section: This section defines key terms used in the policy, such as "Diagnostic Test" and "Hospital Confinement."
If you cannot locate your policy documents or have questions about your coverage, contact your Aflac agent or Aflac's customer service department directly. They can provide you with accurate information about your specific policy and answer any questions you may have.
Important Note: Aflac benefits are designed to supplement, not replace, comprehensive health insurance. They can help with out-of-pocket expenses, but they may not cover the full cost of an MRI or other medical procedures.
Key Takeaways
Here’s a summary of the key points to remember about Aflac's coverage for MRIs:
- Aflac's MRI benefits vary significantly depending on your specific policy type and coverage levels.
- Look for the "Diagnostic Test" benefit in your policy to determine the amount Aflac pays for MRIs.
- If your MRI requires a hospital stay, the "Hospital Confinement" benefit may also apply.
- Waiting periods and pre-existing condition exclusions can affect your eligibility for benefits.
- Submit complete and accurate claims to ensure prompt payment.
- Contact your Aflac agent or customer service for personalized information about your policy.
By understanding the specifics of your Aflac policy, you can better anticipate the benefits you may receive for an MRI and plan accordingly.