Light Therapy for Toenail Fungus: An Overview
Onychomycosis, commonly known as toenail fungus, is a prevalent condition affecting a significant portion of the adult population. Traditional treatments often involve oral antifungal medications or topical solutions, each with varying degrees of success and potential side effects. Light therapy, particularly low-level laser therapy (LLLT), has emerged as a potential alternative or adjunct treatment for toenail fungus. This article provides an overview of light therapy for toenail fungus, focusing on its application in home settings and summarizing the available evidence.
Understanding Light Therapy and its Mechanism
Light therapy, specifically LLLT, involves exposing the affected area to low-intensity light at specific wavelengths. Unlike ablative lasers, LLLT does not generate significant heat or cause tissue destruction. The primary mechanism of action is believed to be photobiomodulation, where light energy is absorbed by cells, leading to a cascade of biological effects. In the context of toenail fungus, LLLT is hypothesized to inhibit fungal growth and potentially stimulate the body's natural defense mechanisms to combat the infection.
It is important to distinguish LLLT from other forms of light therapy, such as ultraviolet (UV) light. UV light is not typically used for toenail fungus due to its potential carcinogenic effects and limited penetration depth. LLLT devices emit light in the red or near-infrared spectrum, which has been shown to have better penetration through the nail plate.
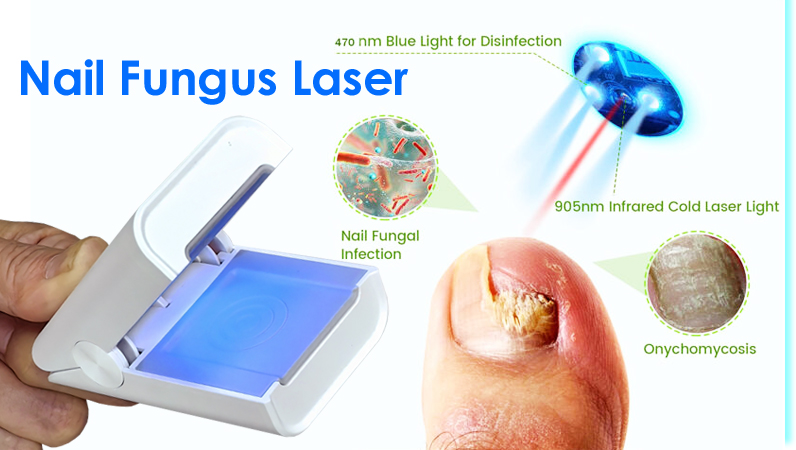
Home-Based Light Therapy Devices
Several light therapy devices are marketed for home use in the treatment of toenail fungus. These devices typically consist of a handheld unit that emits light at a specific wavelength, often around 625nm (red light) or 905nm (near-infrared light). Treatment protocols generally involve applying the device to the affected toenail(s) for a specified duration, ranging from a few minutes to upwards of thirty minutes, on a daily or weekly basis, often for several months. Device manufacturers often recommend combining light therapy with other topical treatments for enhanced efficacy.
The availability of these devices varies depending on the manufacturer and regulatory approval status in different countries. Consumers should be aware that the effectiveness and safety of these devices may not be uniformly established across all brands and models. Before purchasing a device, it is essential to research the manufacturer's credentials, read independent reviews, and consult with a healthcare professional.
Clinical Evidence and Research Findings
The clinical evidence supporting the efficacy of light therapy for toenail fungus is still evolving. Some studies have shown promising results, while others have reported mixed or inconclusive findings. A systematic review and meta-analysis published in the Journal of the American Academy of Dermatology assessed the available evidence and concluded that LLLT might be a beneficial treatment option for onychomycosis, but emphasized the need for more high-quality, randomized controlled trials.
A randomized, double-blind, placebo-controlled trial published in the Journal of Drugs in Dermatology investigated the efficacy of a specific LLLT device for toenail fungus. The study found that the LLLT group showed a statistically significant improvement in nail appearance compared to the placebo group. However, the study also noted that the degree of improvement varied among participants, and complete fungal eradication was not achieved in all cases.
Conversely, some studies have failed to demonstrate a significant benefit of LLLT compared to placebo. These conflicting results highlight the importance of considering factors such as device parameters (wavelength, power density, treatment duration), study design, and patient characteristics when interpreting the available evidence.
Considerations for Home Use
While light therapy devices for toenail fungus are available for home use, it is crucial to use them responsibly and in accordance with the manufacturer's instructions. The following considerations are essential:
Consultation with a Healthcare Professional: Before starting light therapy, it is advisable to consult with a dermatologist or podiatrist to confirm the diagnosis of toenail fungus and discuss the suitability of light therapy as a treatment option.
Proper Device Usage: Follow the manufacturer's instructions carefully regarding treatment duration, frequency, and device placement. Overexposure to light can potentially cause skin irritation or other adverse effects.
Hygiene Practices: Maintain good foot hygiene, including washing and drying feet thoroughly, wearing breathable socks, and disinfecting shoes. These practices can help prevent the spread of fungal infections and enhance the effectiveness of treatment.
Combination Therapy: Light therapy may be more effective when combined with other antifungal treatments, such as topical medications. Discuss the potential benefits of combination therapy with your healthcare provider.
Realistic Expectations: Light therapy may not provide a complete cure for toenail fungus in all cases. Improvement in nail appearance may take several months, and ongoing maintenance may be necessary to prevent recurrence.
Potential Risks and Side Effects
LLLT is generally considered a safe treatment modality, but potential risks and side effects should be considered. The most common side effects are mild and transient, such as skin redness or warmth at the treatment site. In rare cases, more severe reactions, such as blistering or skin discoloration, have been reported. Individuals with photosensitivity or a history of skin cancer should exercise caution and consult with a healthcare professional before using light therapy devices.
The long-term effects of LLLT on the skin and nails are not fully understood. Therefore, it is important to use these devices judiciously and avoid excessive exposure. If any adverse effects occur, discontinue use and seek medical advice.
Alternative and Complementary Therapies
Besides light therapy, several other alternative and complementary therapies are sometimes used for toenail fungus, including tea tree oil, vinegar soaks, and ozone therapy. However, the scientific evidence supporting the efficacy of these therapies is limited, and they should not be considered substitutes for conventional medical treatments. It is crucial to discuss all treatment options with a healthcare professional to determine the most appropriate course of action.
Topical antifungal medications are often recommended in conjunction with other therapies, and may assist in clearing fungal infections more effectively. The active ingredients in these medications vary and each one is often more suitable for particular types of fungal infections. A trained healthcare provider can offer the best advice based on a patient's specific condition.
Key Takeaways
Light therapy, particularly LLLT, represents a potential treatment option for toenail fungus, with home-based devices offering convenience and accessibility. The mechanism of action involves photobiomodulation, which may inhibit fungal growth and stimulate the body's natural defenses.
While some studies have shown promising results, the clinical evidence supporting the efficacy of light therapy for toenail fungus is still evolving. More high-quality, randomized controlled trials are needed to confirm its effectiveness and optimize treatment protocols.
Consumers should exercise caution when selecting and using home-based light therapy devices. Consulting with a healthcare professional, following manufacturer's instructions, maintaining good hygiene practices, and having realistic expectations are essential for maximizing the potential benefits and minimizing the risks. The safety of LLLT is generally good, with only mild skin irritations being the most common complaint.
Light therapy may be more effective when combined with other antifungal treatments, such as topical medications. Alternative and complementary therapies may be considered, but should not replace conventional medical treatments. Individuals are advised to seek guidance from a dermatologist or podiatrist to determine the most appropriate treatment plan for their specific condition.