Okay, so picture this: My grandma, bless her heart, was convinced that putting duct tape on a blister was the ultimate cure. Duct tape! I kid you not. Said it was "tough" and would "protect it." Yeah, protect it from breathing, maybe! Needless to say, it made things infinitely worse. That little blister ended up looking like a science experiment gone wrong. That's when it hit me: skin integrity is a bigger deal than most people realize. And keeping it intact? Well, that's a nursing goal in itself.
So, let's dive into the wonderfully complex (and sometimes slightly gross) world of impaired skin integrity. What is it? Why do we care? And what can nurses, or frankly anyone, do to help?
Understanding Impaired Skin Integrity
Basically, impaired skin integrity means your skin isn't doing its job properly. Your skin is your first line of defense against the outside world. Think of it as your personal, incredibly complex, and self-healing body armor. When that armor is breached – broken, damaged, or compromised – all sorts of nasty things can get in, and important stuff (like fluids!) can leak out. Not ideal.
Impaired skin integrity isn't just a superficial problem. It can lead to:
- Infection: Openings in the skin are like welcome mats for bacteria, viruses, and fungi. And nobody wants a staph infection, trust me.
- Delayed Healing: If your skin's already struggling, any wound you have is going to take longer to heal. We're talking weeks, months, or even years in severe cases.
- Pain and Discomfort: Open wounds can be excruciatingly painful. Even minor skin irritations can be incredibly itchy and uncomfortable. Remember that time you had poison ivy? Enough said.
- Scarring: Impaired skin integrity often leads to scarring, which can be both physically and emotionally distressing.
- Reduced Quality of Life: Chronic wounds and skin conditions can significantly impact a person's ability to perform daily activities, socialize, and enjoy life.
So, yeah, it's kind of a big deal. Don't underestimate the power of healthy skin!
Common Causes of Impaired Skin Integrity
There are tons of reasons why someone might experience impaired skin integrity. It's not always just bad luck. Some common culprits include:
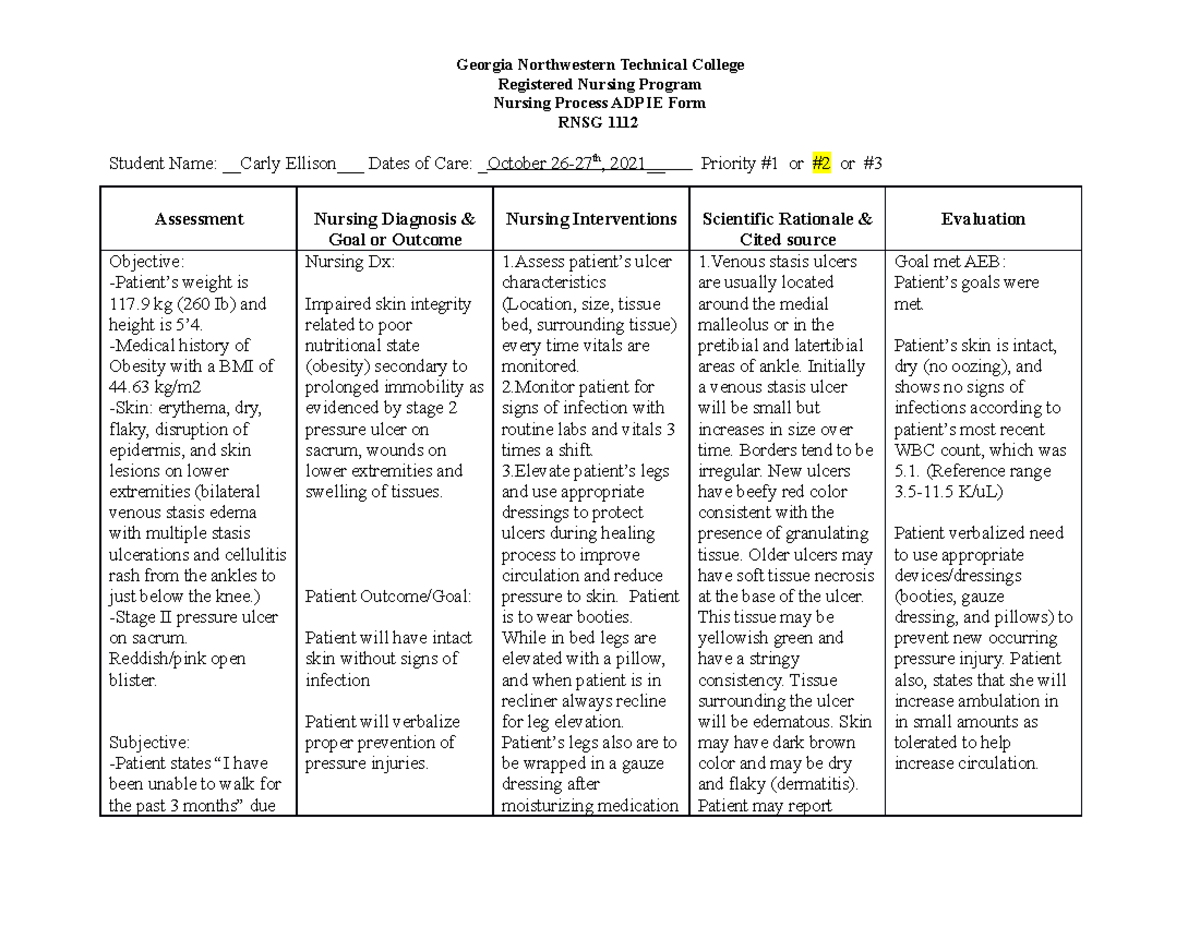
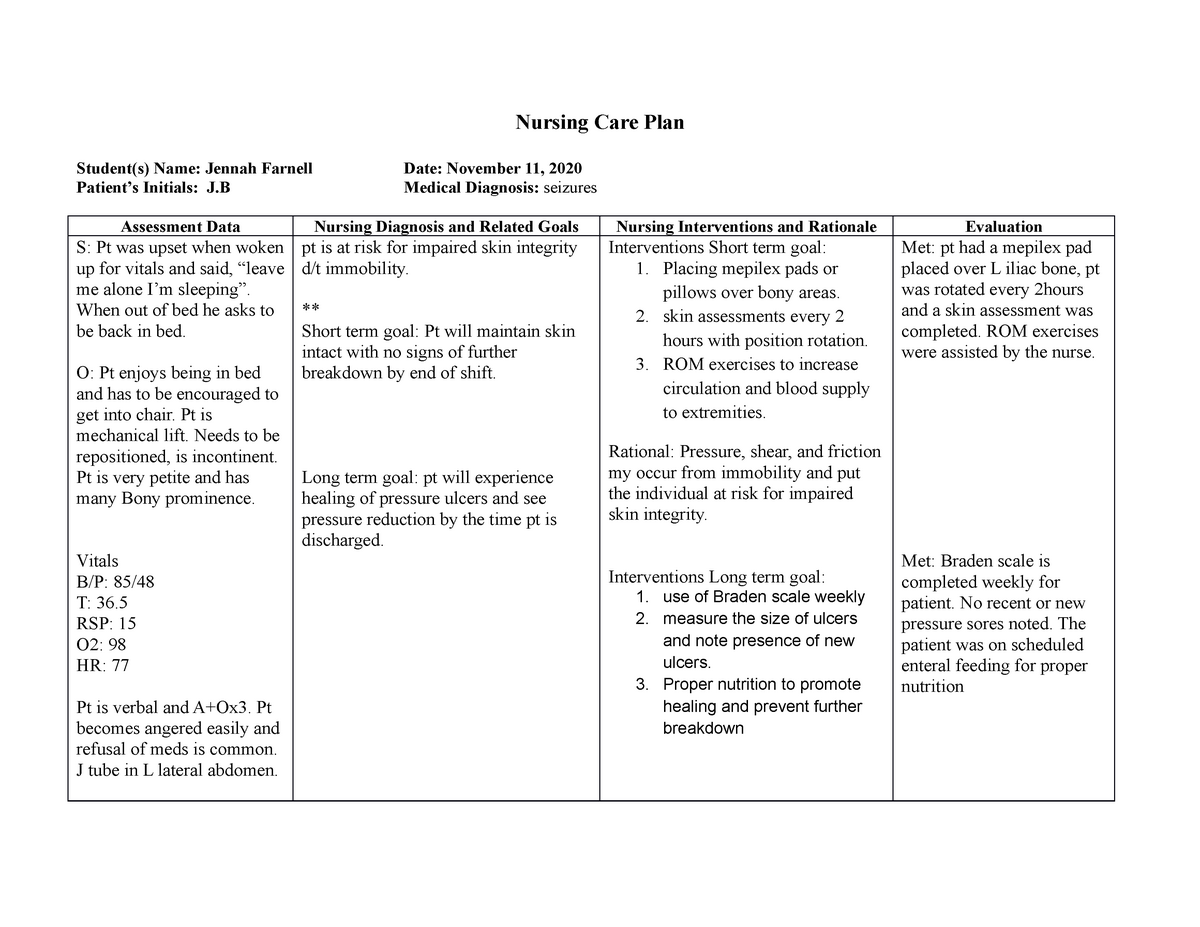
- Pressure: Prolonged pressure on one area, like from sitting or lying in the same position for too long, can cut off blood flow and lead to pressure ulcers (bedsores). This is a major concern for bedridden patients.
- Moisture: Too much moisture (like from sweat, urine, or wound drainage) can soften the skin and make it more susceptible to breakdown. Think of leaving your hands in water for too long – that wrinkly, fragile feeling? Now imagine that constantly.
- Friction and Shear: Friction (rubbing) and shear (when skin layers slide against each other) can damage the skin. Things like sliding down in bed or wearing ill-fitting shoes can cause this.
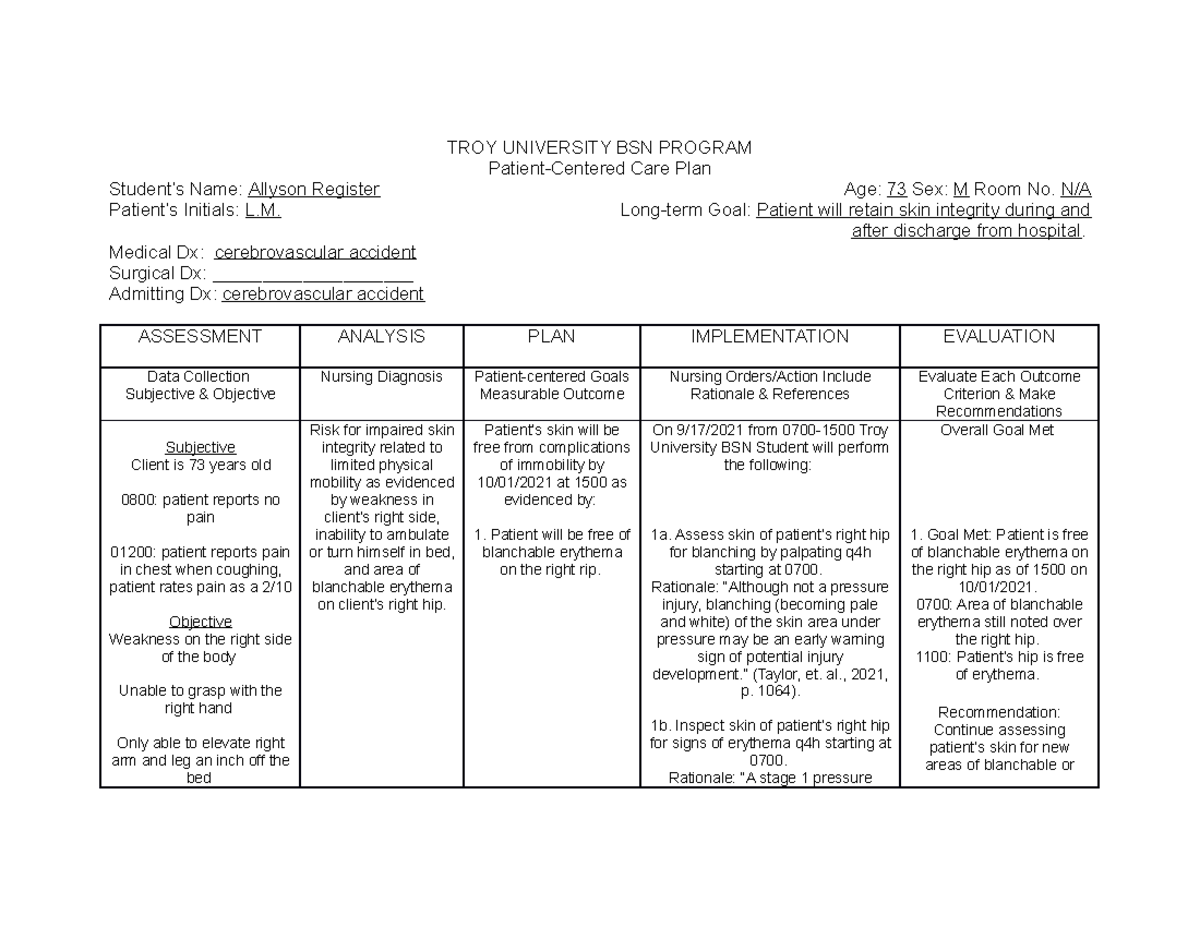
- Immobility: Reduced mobility increases the risk of pressure ulcers, as people are unable to shift their weight and relieve pressure points.
- Poor Nutrition: Healthy skin needs proper nutrients to function and repair itself. Malnutrition can weaken the skin and make it more vulnerable to injury. Are you getting enough vitamins and minerals? I'm just asking...
- Age: As we age, our skin becomes thinner, drier, and less elastic. This makes it more prone to injury and slower to heal. The fountain of youth is still undiscovered, unfortunately.
- Medical Conditions: Certain medical conditions, such as diabetes, vascular disease, and immune disorders, can impair skin integrity.
- Medications: Some medications can have side effects that affect the skin, such as thinning the skin or making it more sensitive to sunlight.
- Radiation Therapy: Radiation therapy can damage the skin in the treated area.
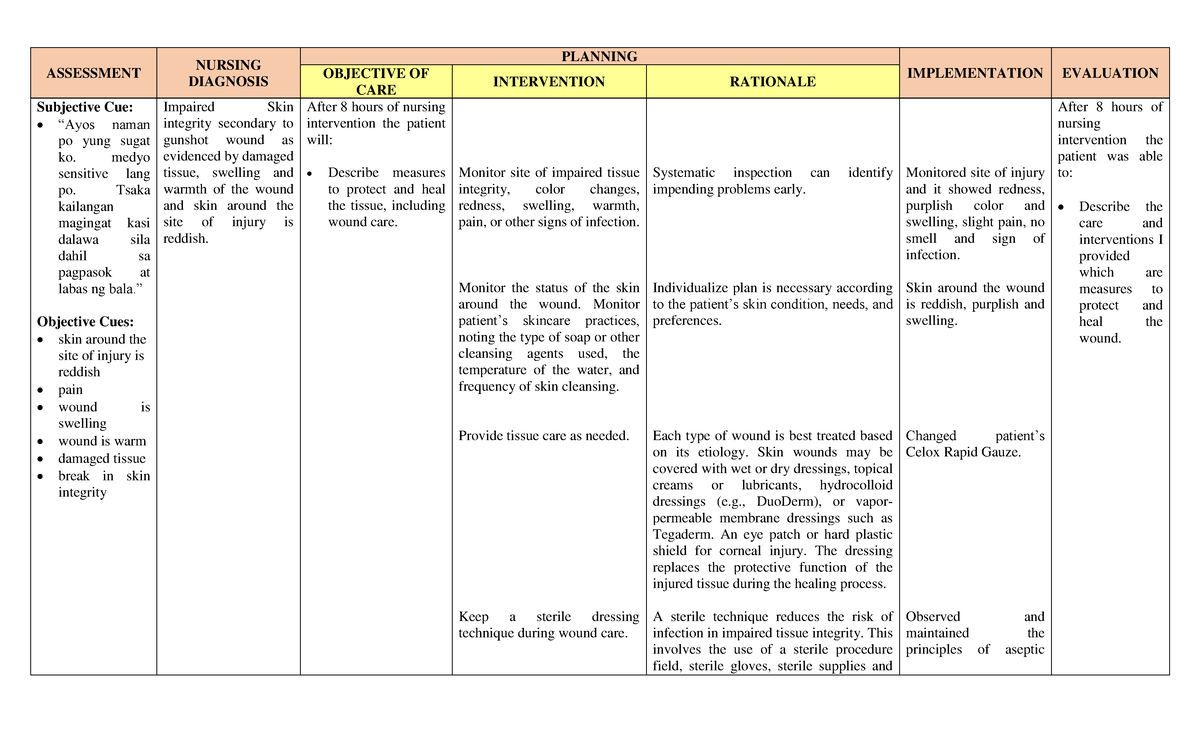
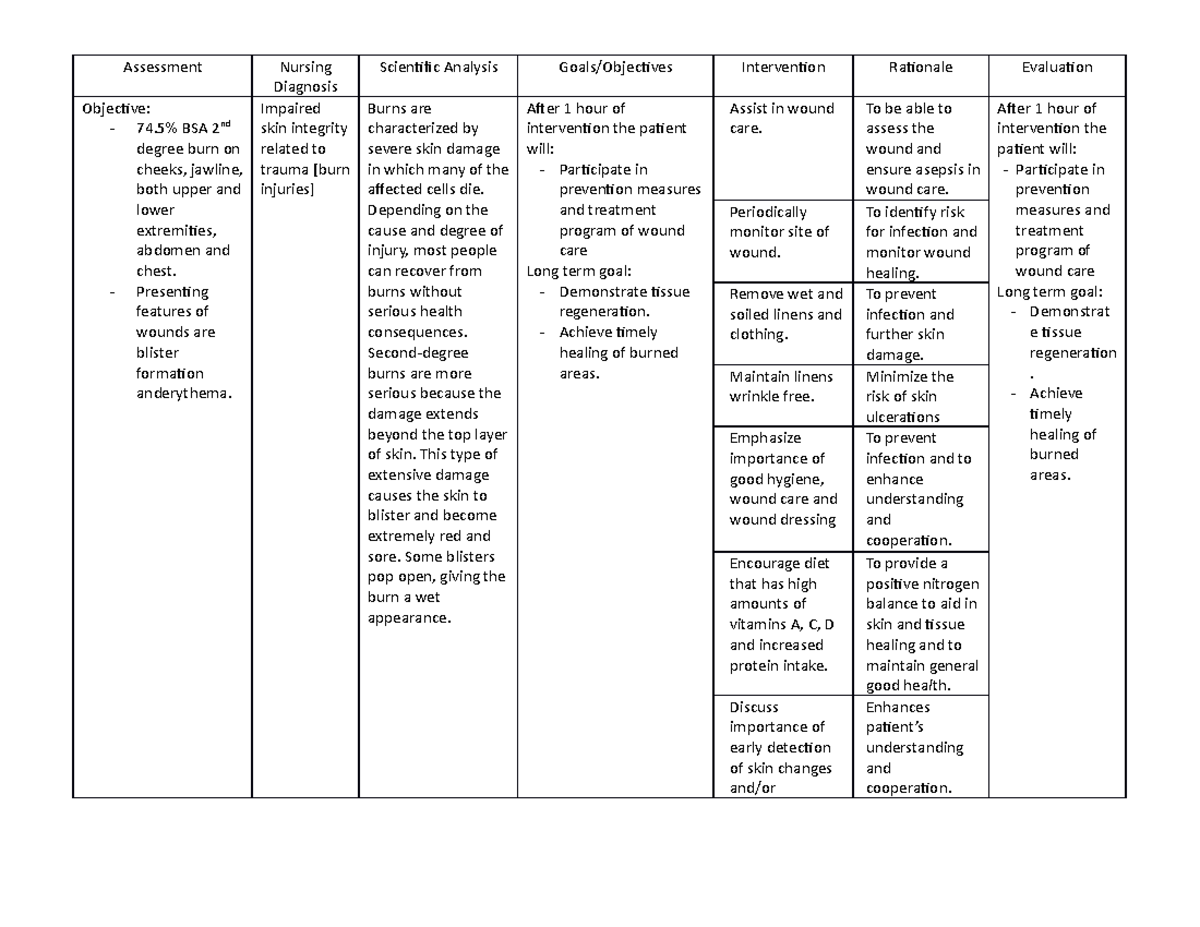
- Trauma: Injuries like cuts, burns, and abrasions can obviously disrupt skin integrity.
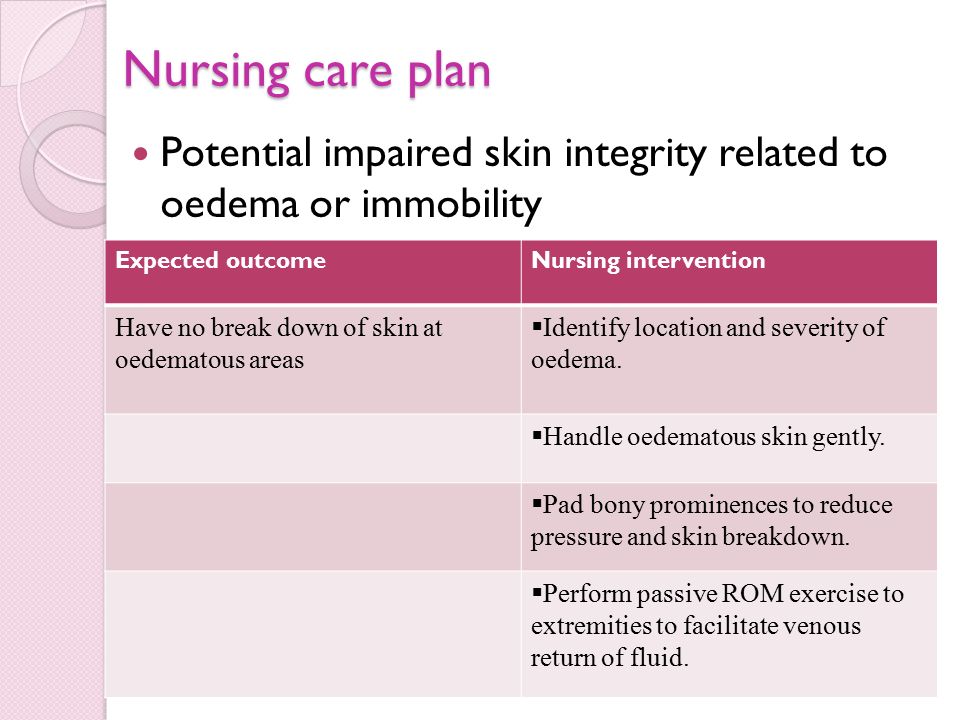
The Nursing Goal: Protecting and Restoring Skin Integrity
Okay, so we know what impaired skin integrity is and why it's a problem. Now, what's a nurse to do? Well, the primary nursing goal is to prevent skin breakdown in the first place and, if it's already happened, to promote healing.
This involves a multi-faceted approach that includes:
Risk Assessment
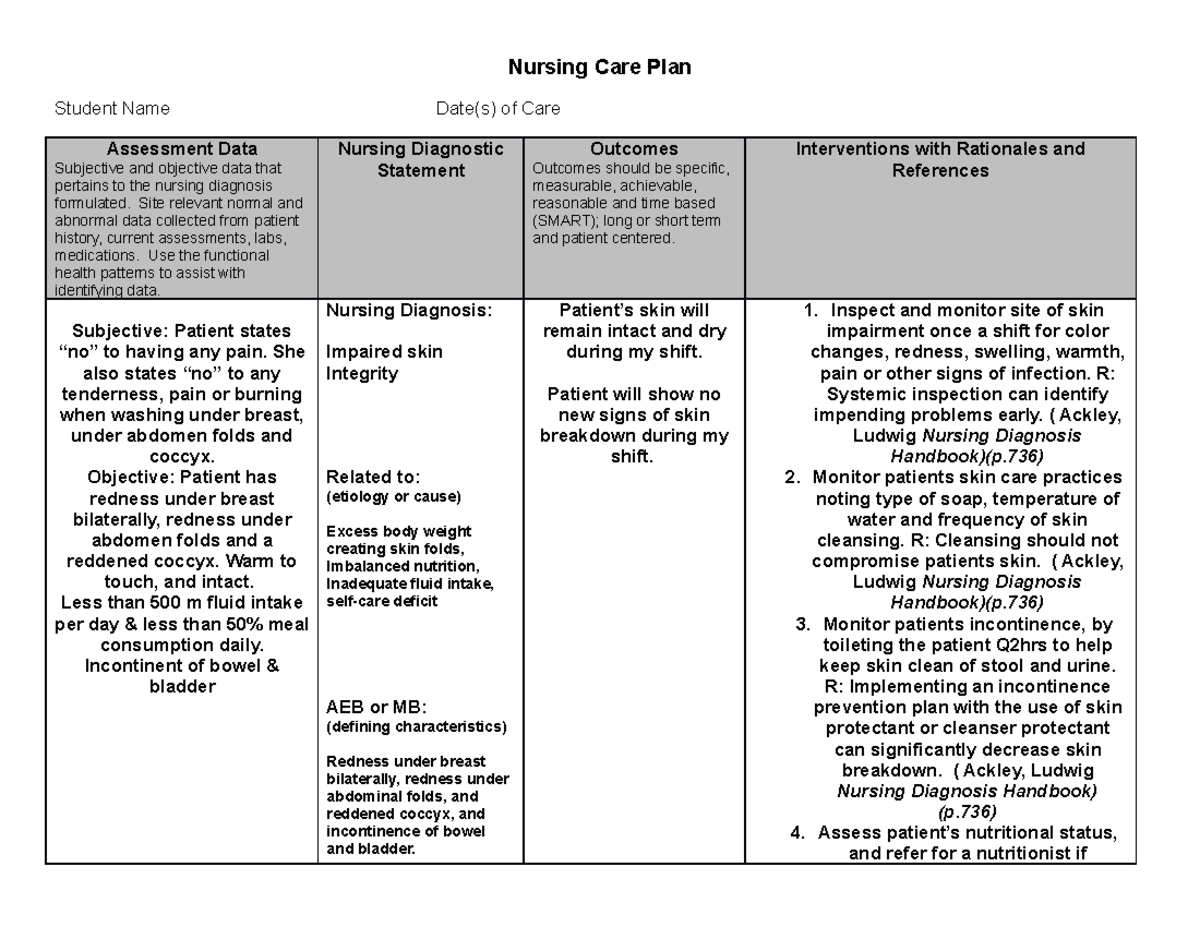
The first step is identifying patients who are at risk for developing skin problems. This involves a thorough assessment of their:
- Medical History: What medical conditions do they have? What medications are they taking?
- Mobility: How mobile are they? Can they move around independently, or do they need assistance?
- Nutritional Status: Are they getting enough calories and nutrients? Are they able to eat and drink adequately?
- Skin Condition: What does their skin look like? Are there any existing areas of redness, dryness, or breakdown?
- Continence: Are they incontinent of urine or stool? (This is a delicate topic, but very important for skin health!)
Nurses often use standardized risk assessment tools, such as the Braden Scale, to help them identify patients at risk for pressure ulcers. These scales assess factors like sensory perception, moisture, activity, mobility, nutrition, and friction/shear.
Pro Tip: It is better to be proactive than reactive.
Prevention Strategies
Once a patient's risk level has been determined, the nurse can implement appropriate prevention strategies. These might include:
- Frequent Repositioning: Repositioning patients at regular intervals (usually every two hours) helps to relieve pressure on bony prominences. Think of it like rotating your tires – you want to distribute the wear evenly.
- Pressure-Relieving Devices: Using special mattresses, cushions, and heel protectors can help to reduce pressure on vulnerable areas. These devices distribute weight more evenly and provide cushioning.
- Skin Care: Keeping the skin clean and dry is essential. This involves gentle cleansing with mild soap and water, followed by thorough drying. Moisturizing the skin regularly can also help to prevent dryness and cracking.
- Incontinence Management: Promptly cleaning and drying the skin after episodes of incontinence is crucial. Barrier creams can also be used to protect the skin from moisture.
- Nutrition and Hydration: Ensuring that patients are getting adequate nutrition and hydration is vital for maintaining skin health. A diet rich in protein, vitamins, and minerals can help to promote skin repair.
- Education: Educating patients and their families about the importance of skin care and prevention strategies is essential. They need to understand how to protect their skin and what to look for.
Wound Care
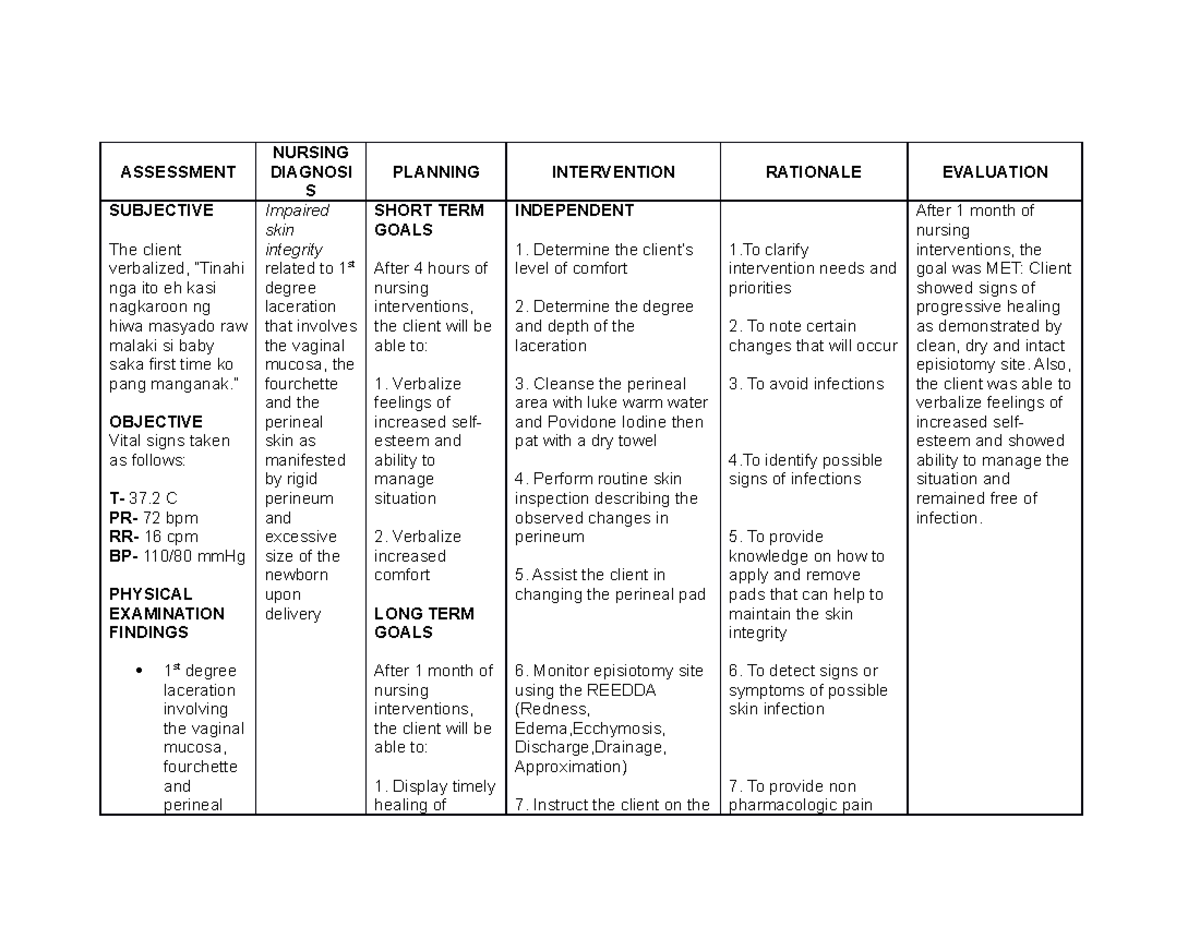
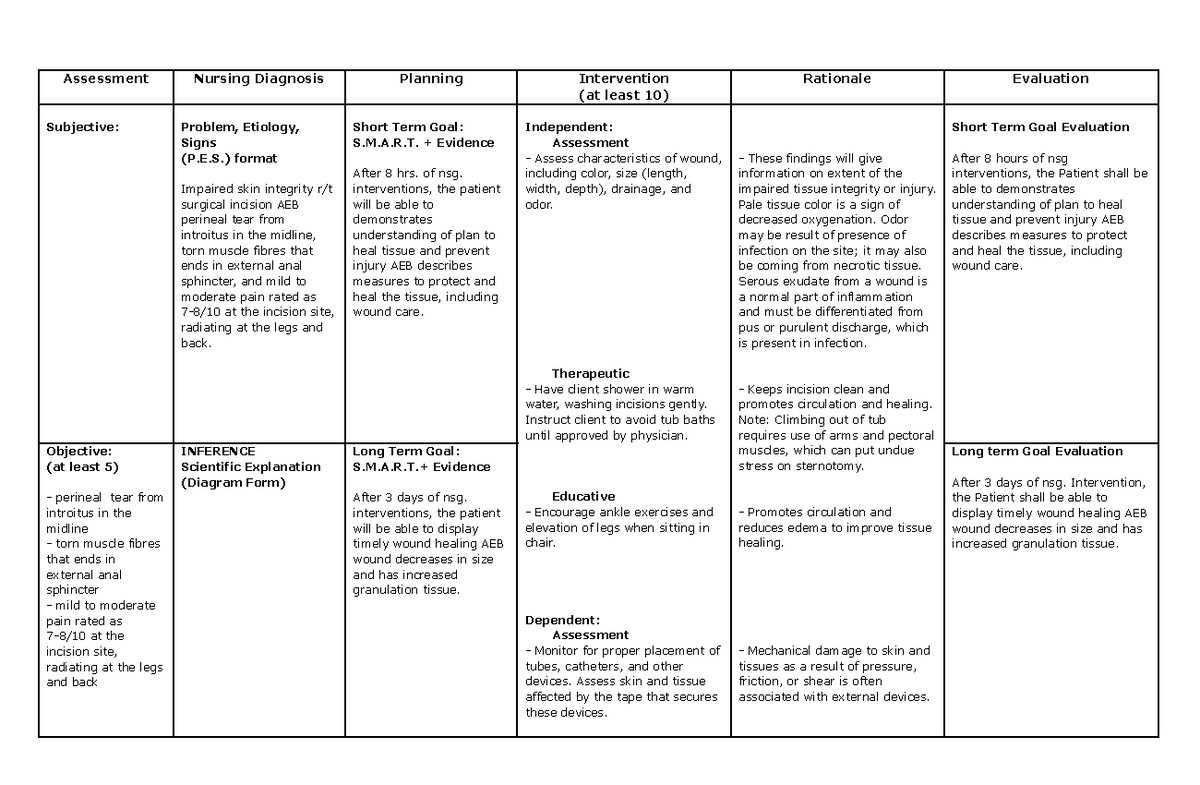
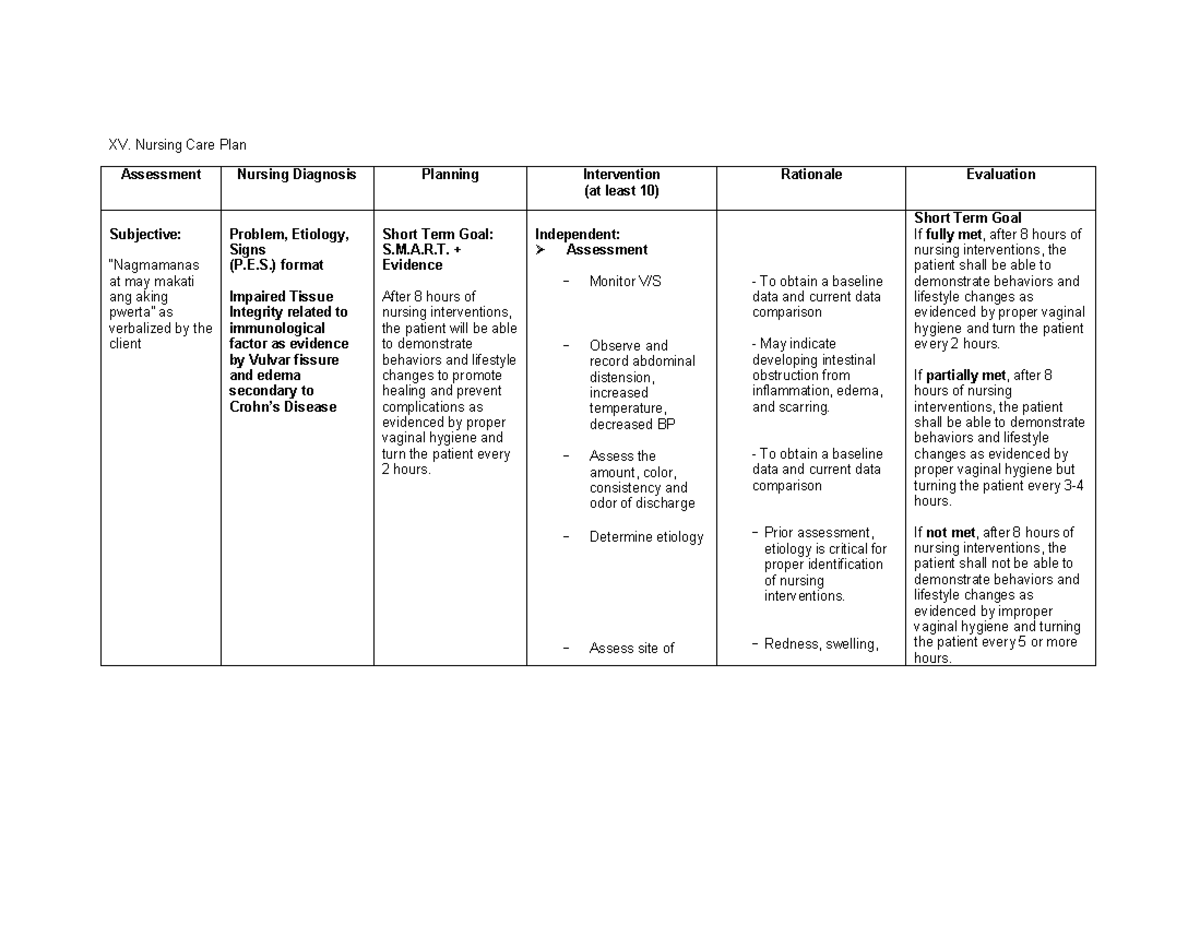
If a patient already has impaired skin integrity, the nurse's focus shifts to promoting wound healing. This involves:
- Wound Assessment: Regularly assessing the wound to monitor its size, depth, and appearance. Documenting these findings is crucial for tracking progress.
- Wound Cleansing: Cleaning the wound to remove debris and bacteria. The type of cleansing solution used will depend on the type of wound.
- Debridement: Removing dead or damaged tissue from the wound. This can be done surgically, mechanically, chemically, or autolytically (using the body's own enzymes).
- Wound Dressing: Applying a dressing to protect the wound and promote healing. There are many different types of wound dressings available, each with its own advantages and disadvantages. The choice of dressing will depend on the type of wound, its location, and the amount of drainage.
- Pain Management: Managing pain associated with the wound. This may involve medications, positioning, or other comfort measures.
- Infection Control: Preventing infection by using sterile technique when changing dressings and monitoring for signs of infection.
- Nutritional Support: Ensuring that the patient is getting adequate nutrition to support wound healing.
Wound care can be complex and challenging. Nurses often work with wound care specialists to develop individualized treatment plans for patients with complex wounds.
Documentation is Key
If it wasn't documented, it didn't happen! I cannot stress this enough. Meticulous documentation is essential for monitoring progress, communicating with other healthcare providers, and ensuring that patients receive the best possible care. Nurses should document:
- Risk Assessments: The results of risk assessments, including the Braden Scale score.
- Skin Assessments: The condition of the patient's skin, including any areas of redness, dryness, or breakdown.
- Wound Assessments: The size, depth, appearance, and drainage of any wounds.
- Interventions: All interventions performed to prevent or treat impaired skin integrity, such as repositioning, skin care, and wound dressing changes.
- Patient Education: Any education provided to the patient and their family.
- Outcomes: The patient's response to treatment and any changes in their skin condition.
More Than Just a Job: Compassion and Empathy
Taking care of patients with impaired skin integrity is not just about applying dressings and following protocols. It's also about providing compassionate and empathetic care. Many patients with skin problems experience pain, discomfort, and social isolation. Nurses need to be sensitive to these challenges and provide emotional support.
Think about it: having a large, open wound can be incredibly embarrassing and distressing. Patients may be afraid to show their wound to others or participate in social activities. Nurses can help by creating a safe and supportive environment where patients feel comfortable discussing their concerns.
Being empathetic goes a long way.
So, What Can *You* Do?
Okay, so maybe you're not a nurse. But that doesn't mean you can't play a role in preventing and managing impaired skin integrity! Here are a few things you can do:
- If you're caring for a loved one at home: Learn about pressure ulcers and other skin problems. Talk to their doctor or nurse about how to prevent them. Make sure they're getting enough nutrition and hydration. Help them to reposition regularly.
- If you're a patient in a hospital or nursing home: Don't be afraid to speak up if you're uncomfortable or if you notice any changes in your skin. Ask for help with repositioning. Make sure you're getting enough to eat and drink.
- Everyone: Take care of your own skin! Stay hydrated, eat a healthy diet, and protect your skin from the sun. And for goodness sake, don't put duct tape on blisters! (Just kidding... mostly.)
Ultimately, protecting and restoring skin integrity is a team effort. By working together, we can help to prevent suffering and improve the quality of life for people of all ages.
And remember, even small acts of kindness and compassion can make a big difference in someone's life. So, go out there and be a skin-saving superhero! (Okay, maybe that's a bit much. But you get the idea.)