Okay, let's talk about something seriously cool. Something that could potentially change lives in a major way – stem cell therapy for diabetes! Now, I know what you might be thinking: "Stem cells? Sounds like science fiction!" And yeah, it *does* sound a bit futuristic, but trust me, it's becoming more and more of a reality. And for those living with diabetes, that's incredibly exciting news.
Diabetes, as you probably know, is a tough cookie. It messes with your body's ability to regulate blood sugar, and that can lead to all sorts of problems. Managing it can feel like a full-time job – constant monitoring, insulin injections, dietary restrictions... it can be exhausting! But what if there was a way to *actually address the root cause* of the problem, instead of just managing the symptoms? Enter stem cell therapy. (Cue dramatic music!).
What's the Big Deal with Stem Cells, Anyway?
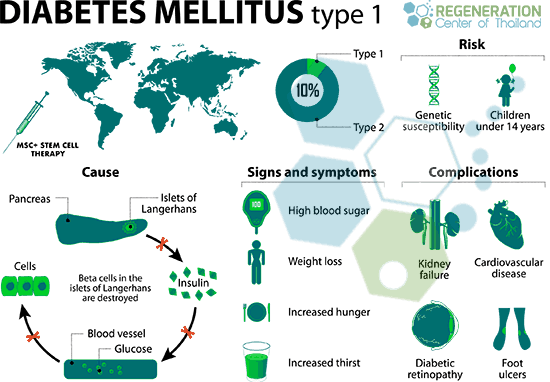
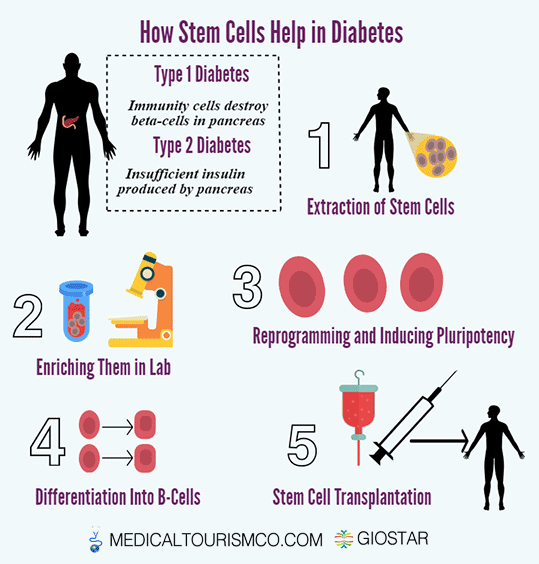
So, what exactly are stem cells? Well, imagine them as the body's super-powered repair crew. They're like blank slates, capable of transforming into different types of cells – and that includes the all-important insulin-producing cells in your pancreas, known as beta cells. In type 1 diabetes, the body's immune system mistakenly attacks and destroys these beta cells. In type 2, the cells become resistant to insulin. Either way, it's a problem. Stem cell therapy aims to fix this by either replacing the damaged cells or protecting the existing ones.
Think of it like this: your pancreas is a factory that makes insulin. In diabetes, that factory is either broken down (type 1) or inefficient (type 2). Stem cells, potentially, are the construction workers who can rebuild or repair that factory. Pretty amazing, right?
Stem Cell Therapy: How Does It Work?
There are a few different approaches to stem cell therapy for diabetes, and research is constantly evolving (which is a good thing!). Here are a couple of the main methods:
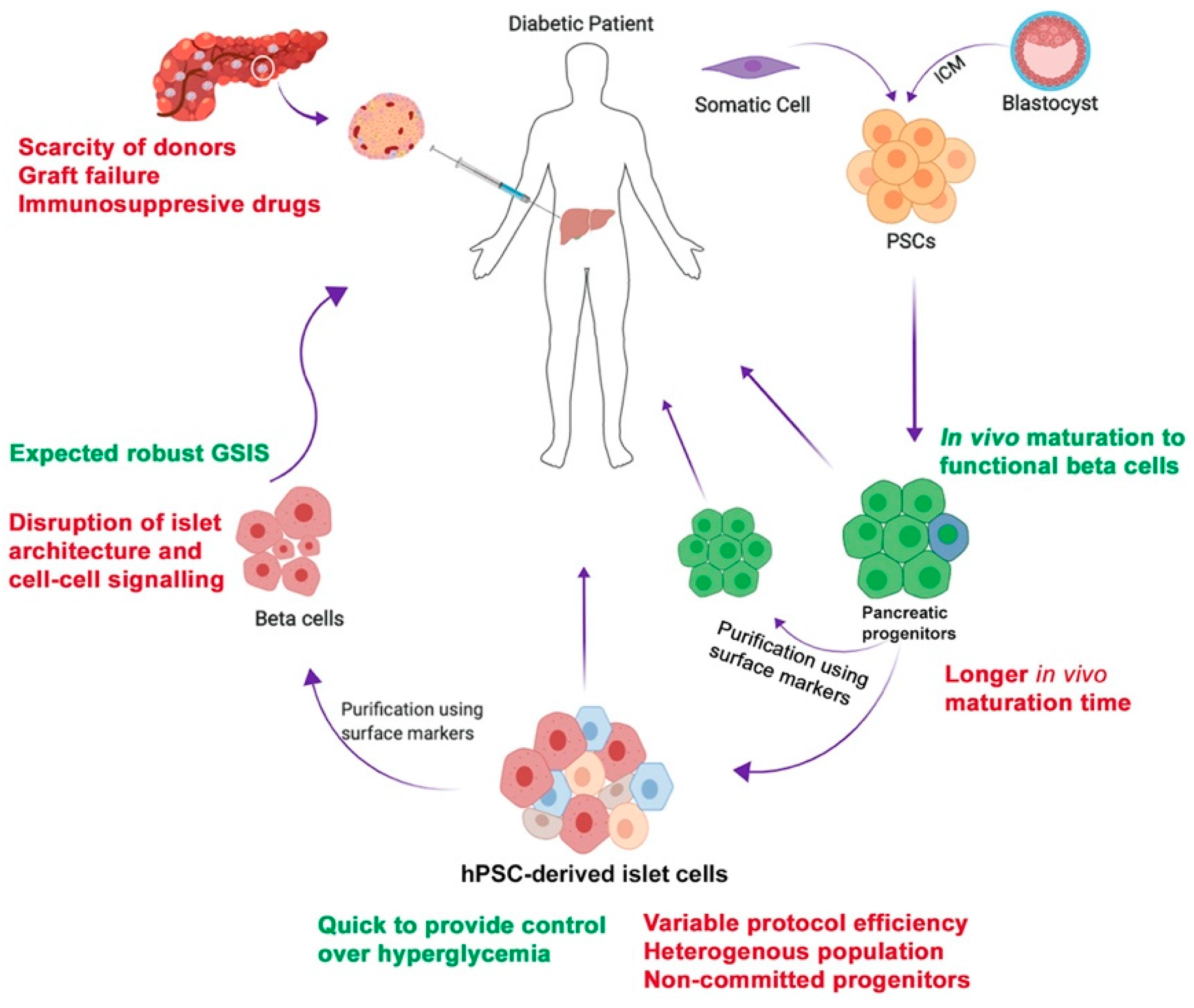
Replacing Damaged Beta Cells
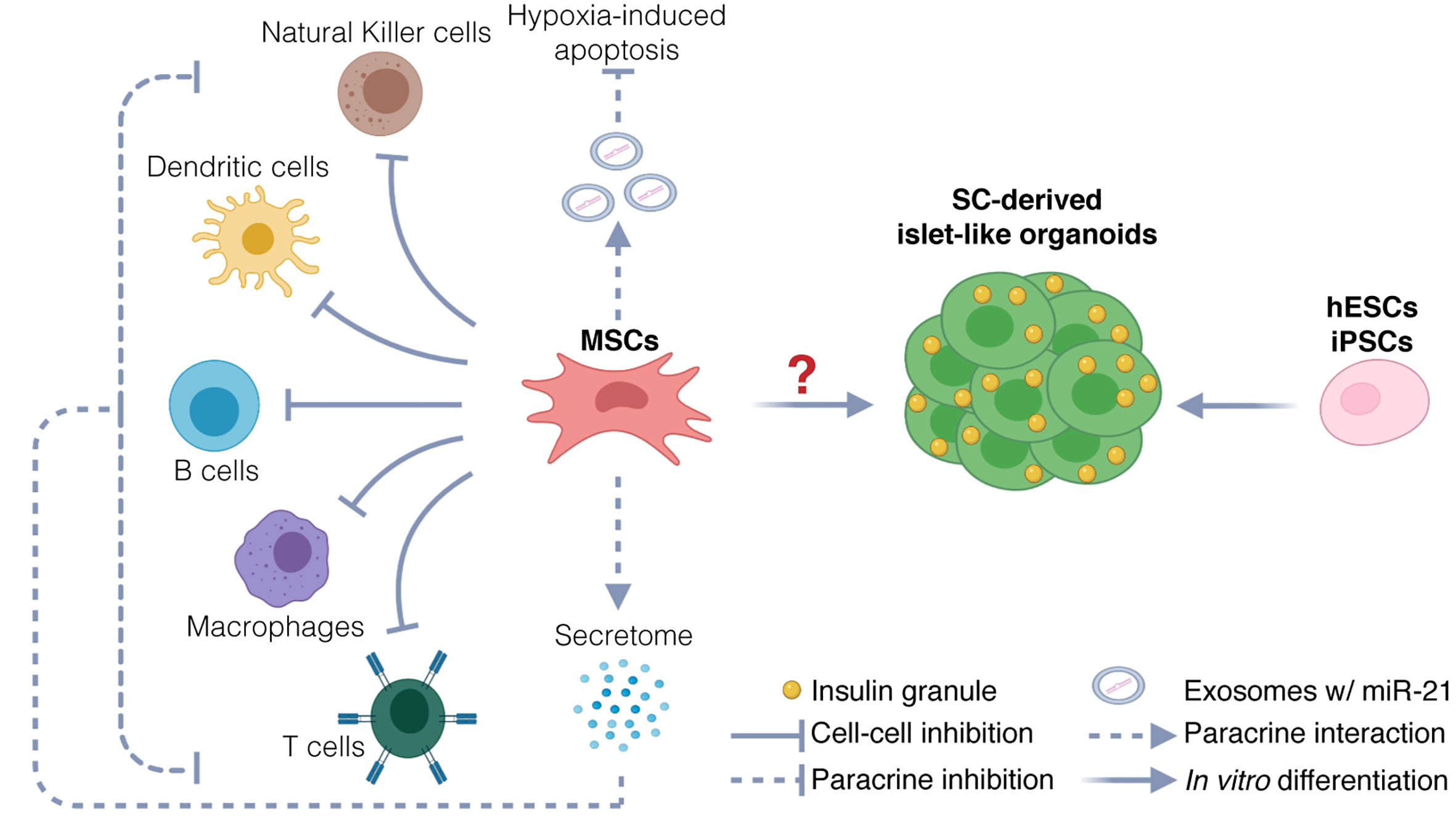
One strategy focuses on replacing the destroyed beta cells in type 1 diabetes. Scientists take stem cells (often from the patient themselves, which reduces the risk of rejection - clever, eh?) and coax them into becoming beta cells in the lab. These new beta cells are then transplanted back into the patient, where they hopefully start producing insulin again. The goal? To reduce or even eliminate the need for insulin injections. Imagine the freedom!
Protecting Existing Beta Cells
Another approach aims to protect the existing beta cells from further damage, especially in the early stages of type 1 diabetes. Stem cells can release factors that suppress the immune system, preventing it from attacking the beta cells. It's like sending in a security force to protect the insulin factory from being vandalized. This can potentially slow down or even halt the progression of the disease.
Improving Insulin Sensitivity
For Type 2 diabetes, some therapies focus on enhancing insulin sensitivity. Certain stem cells have the power to secrete factors that improve how the body uses the insulin it produces. This may reduce insulin resistance and help regulate blood sugar levels.
Okay, But What About the Success Rate? Let's Talk Numbers!
Alright, alright, I know what you're really here for. The million-dollar question: What's the success rate? And here's where it gets a little tricky. Because stem cell therapy for diabetes is still a relatively new field, the data is still being gathered. Also, *success* can mean different things to different people. Does it mean a complete cure? A significant reduction in insulin needs? Better blood sugar control?
Here's what we *do* know:
- Early Clinical Trials Show Promise: Several clinical trials have shown encouraging results, with some patients experiencing a significant reduction in their need for insulin, and others even becoming insulin-independent for a period of time. That's HUGE!
- Success Varies: The success rate can vary depending on a number of factors, including the type of diabetes (type 1 or type 2), the stage of the disease, the patient's overall health, and the specific type of stem cell therapy used. Think of it like baking a cake – lots of ingredients and variables can impact the final result.
- Long-Term Data is Still Emerging: While the short-term results of some trials are positive, we need more long-term data to fully understand the durability of the treatment and its potential side effects. Like any new technology, there is still a learning curve.
It's important to remember that stem cell therapy is not a guaranteed cure for diabetes *yet*. But the progress that's being made is incredibly exciting, and the potential for future breakthroughs is enormous. We are talking about potentially revolutionizing the way we manage (and maybe even cure!) this disease.
The Importance of Reputable Research and Treatment
Now, a word of caution. Because stem cell therapy is still a relatively new field, there are a lot of clinics out there offering unproven and potentially dangerous treatments. It's absolutely crucial to do your research and choose a reputable clinic with experienced doctors and a strong track record. Don't fall for miracle cures or clinics that promise unrealistic results. If it sounds too good to be true, it probably is!
Look for clinics that are conducting rigorous clinical trials and publishing their results in peer-reviewed journals. Talk to your doctor or a diabetes specialist about whether stem cell therapy might be right for you, and get their advice on finding a qualified provider. Your health and safety should always be your top priority.
Potential Risks and Side Effects
Like any medical procedure, stem cell therapy carries some potential risks and side effects. These can include:
- Rejection of the transplanted cells: This is a risk with any transplant procedure, but can be minimized by using the patient's own stem cells.
- Infection: Any invasive procedure carries a risk of infection.
- Tumor formation: In rare cases, stem cells can potentially form tumors.
- Immune system complications: Stem cell therapy can affect the immune system, potentially leading to autoimmune reactions.
It's important to discuss these risks with your doctor before considering stem cell therapy. A thorough understanding of the potential benefits and risks is essential for making an informed decision.
Living a Fuller Life with Better Diabetes Management
Let's face it: managing diabetes can be a real drag. It can impact your energy levels, your diet, your social life, and your overall sense of well-being. But imagine a future where you could spend less time worrying about your blood sugar and more time doing the things you love. Hiking in the mountains? Traveling the world? Playing with your grandkids? The possibilities are endless! While stem cell therapy is not the only thing you can do to achieve this, it does have the potential to be a vital part of it.
That's what's so exciting about the potential of stem cell therapy for diabetes. It's not just about managing a disease; it's about restoring quality of life. It's about giving people back their freedom, their energy, and their sense of control. Who wouldn't want that?
Looking Ahead: The Future of Stem Cell Therapy for Diabetes
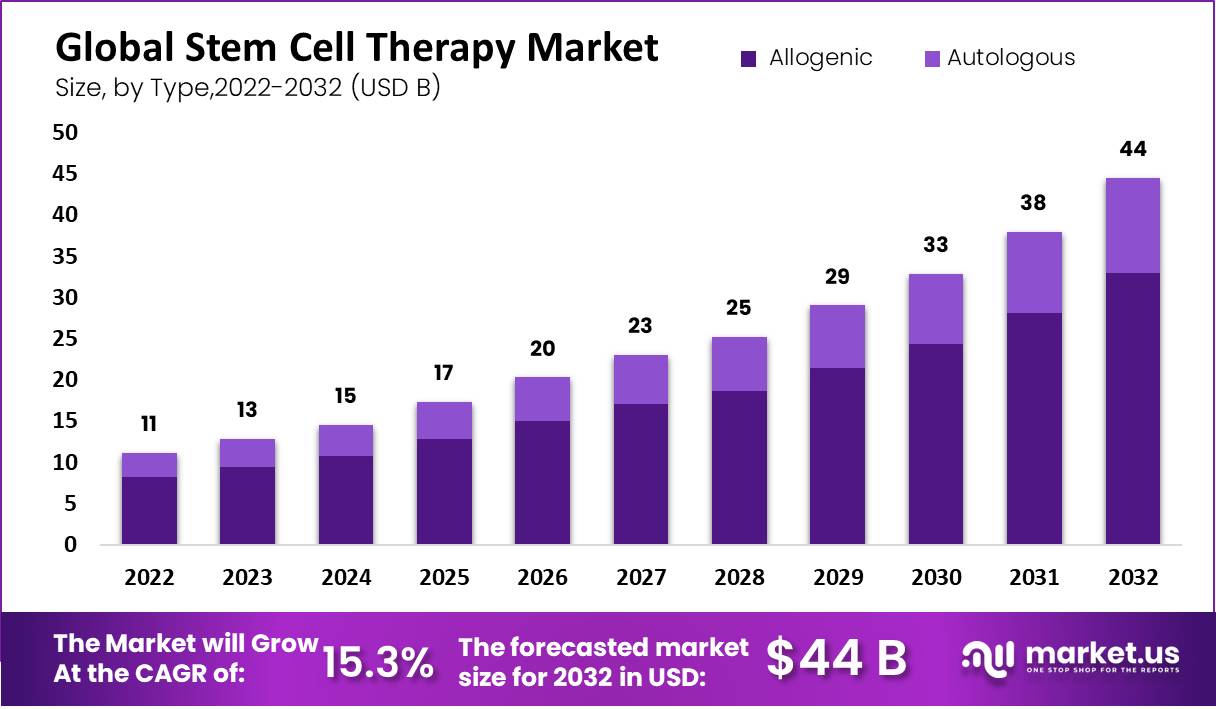
The field of stem cell therapy is rapidly evolving, and we can expect to see even more advancements in the coming years. Researchers are exploring new sources of stem cells, developing more efficient methods for differentiating them into beta cells, and finding ways to protect the transplanted cells from immune attack. The future looks bright!
One of the most exciting areas of research is the development of encapsulation devices that can protect the transplanted beta cells from the immune system without the need for immunosuppressant drugs. These devices are like tiny shields that allow the beta cells to function normally while preventing the immune system from attacking them. It's like giving those construction workers special protective gear!
Another promising area is the use of gene editing technologies like CRISPR to modify stem cells and make them more resistant to immune attack. This could potentially eliminate the need for immunosuppressant drugs altogether.
So, What Can You Do?
Even though stem cell therapy for diabetes is still in its early stages, there are things you can do to stay informed and advocate for progress:
- Stay informed: Keep up with the latest research and clinical trials. Reputable organizations like the American Diabetes Association and the Juvenile Diabetes Research Foundation (JDRF) are good sources of information.
- Talk to your doctor: Discuss your interest in stem cell therapy and get their perspective on whether it might be right for you.
- Support research: Donate to organizations that are funding research into stem cell therapy for diabetes.
- Advocate for policy changes: Encourage your elected officials to support policies that promote stem cell research and make these therapies more accessible to patients.
Ultimately, the future of stem cell therapy for diabetes depends on continued research, collaboration, and advocacy. By working together, we can help make this promising therapy a reality for millions of people living with diabetes.
The information in this article is not intended to be a substitute for professional medical advice. Always talk to your doctor about any health concerns or before making any decisions about your treatment plan.
Stem cell therapy is not without its detractors. Concerns have been voiced over ethical considerations regarding the use of embryonic stem cells (though research increasingly focuses on adult stem cells and induced pluripotent stem cells to bypass these concerns), the potential for unregulated clinics offering unproven treatments, and the need for more rigorous clinical trials to establish efficacy and safety. It's important to approach the topic with a critical and informed perspective, seeking out diverse sources of information and consulting with qualified medical professionals.
Remember, knowledge is power. The more you learn about stem cell therapy, the better equipped you'll be to make informed decisions about your health and to advocate for progress in this exciting field. So, go out there, do your research, and get involved! The future of diabetes treatment may just be in your hands.
I hope this has inspired you, now, go out there and change the world!