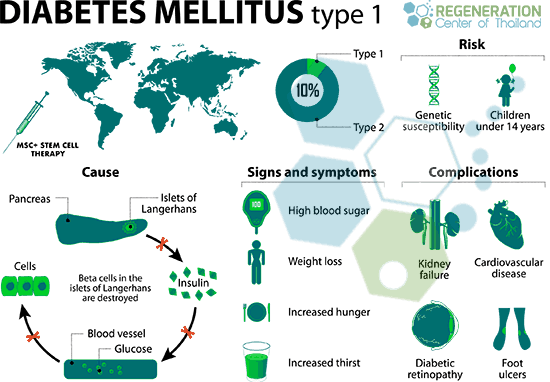
Type 2 diabetes (T2D) is a chronic metabolic disorder affecting millions worldwide. While traditional treatments like lifestyle changes, oral medications, and insulin injections can manage the condition, they often don't address the underlying cause of insulin resistance. Stem cell therapy has emerged as a potential regenerative approach, offering hope for improved glycemic control and even potential remission in some cases. Understanding the success rates, limitations, and what to expect from stem cell therapy is crucial for individuals considering this treatment option.
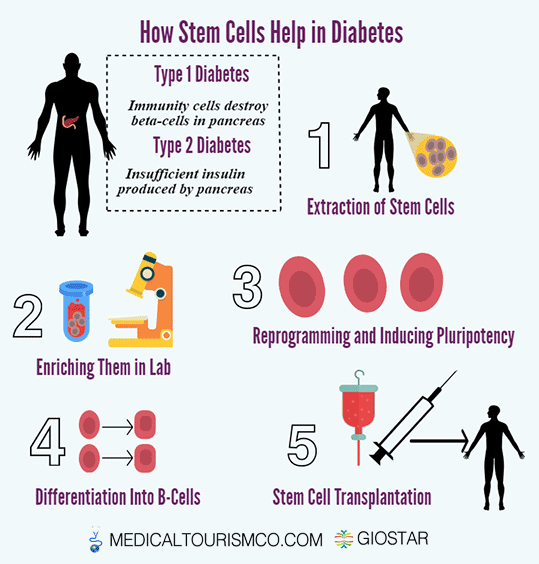
Understanding Stem Cell Therapy for Type 2 Diabetes
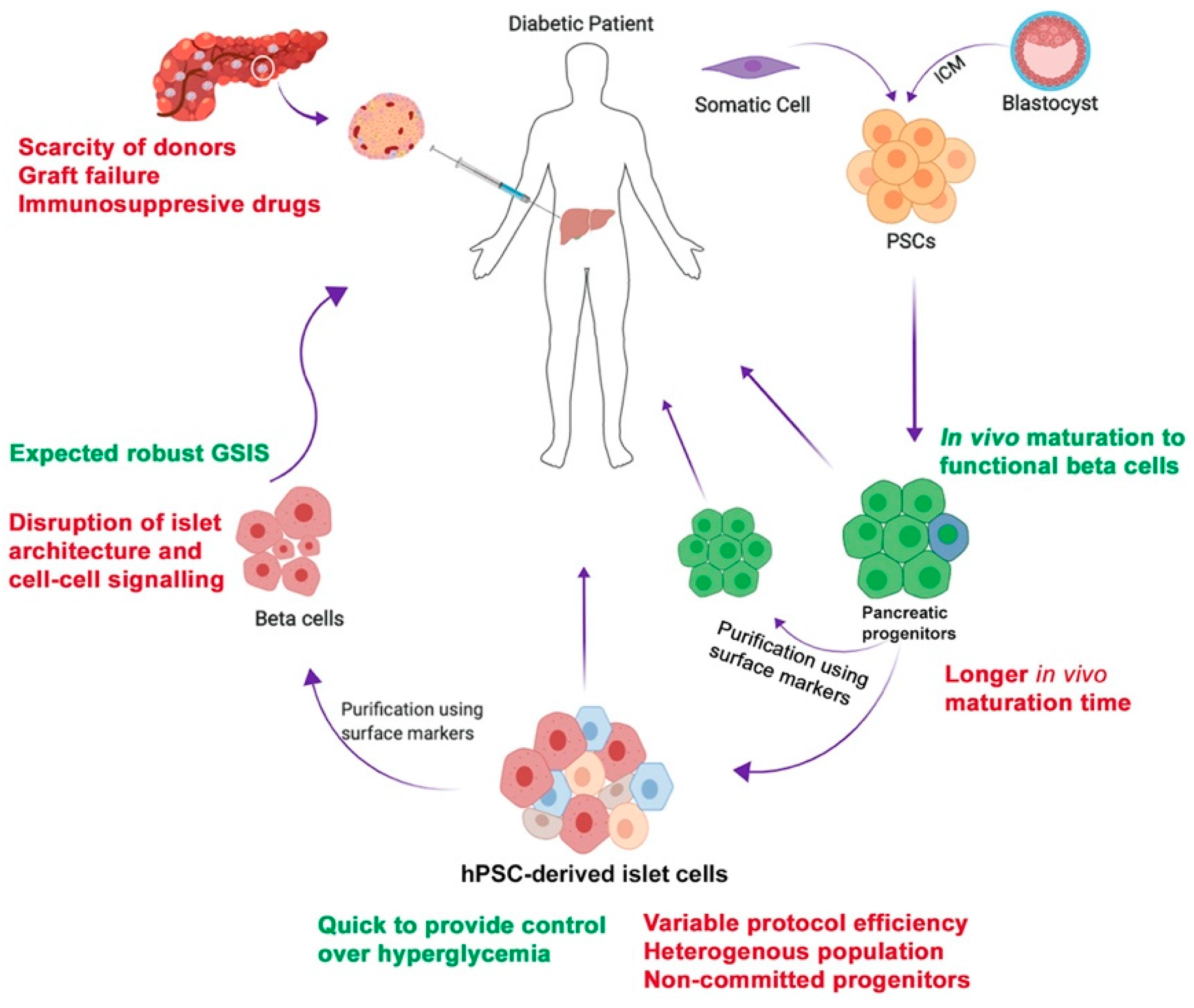
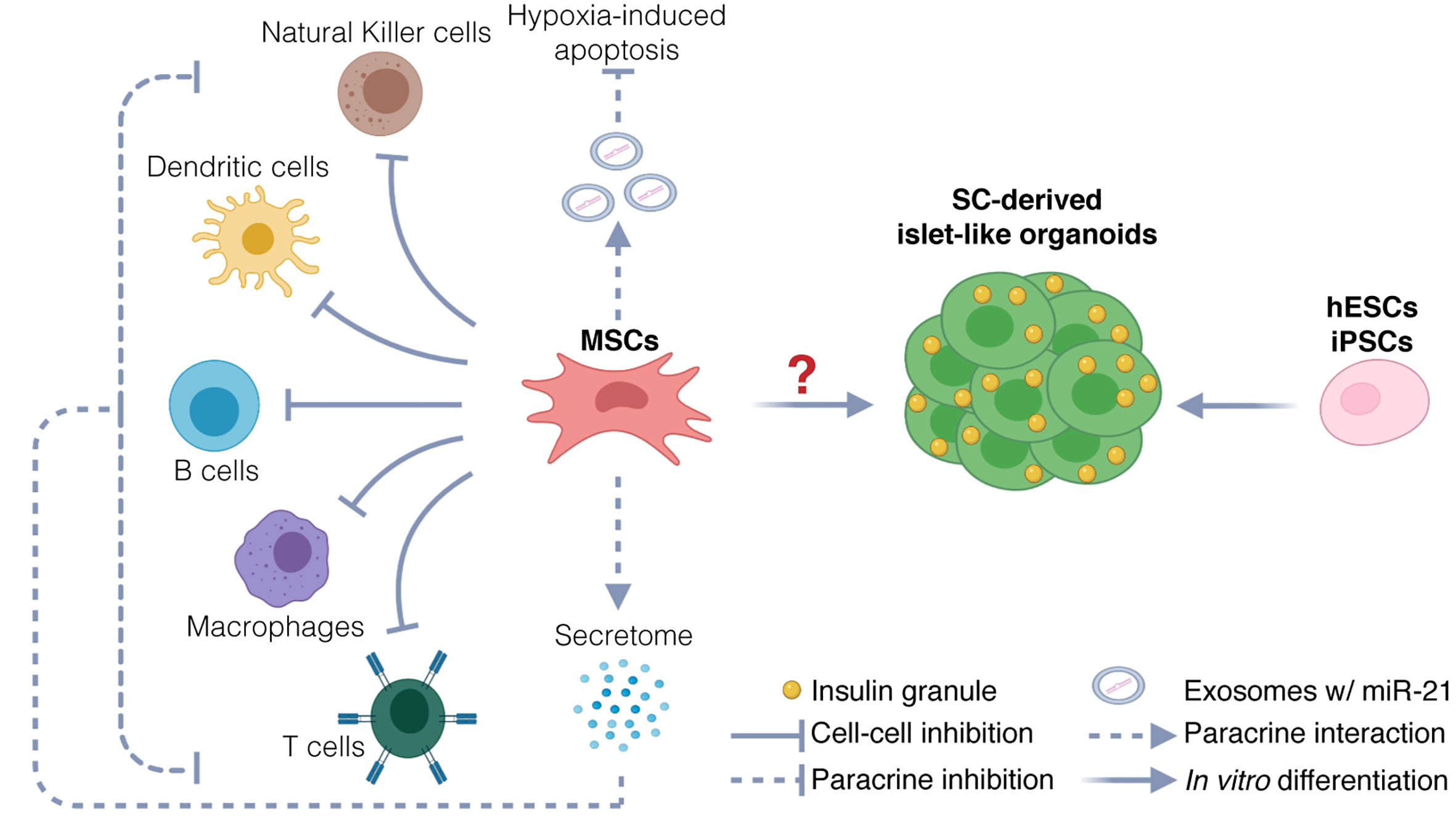
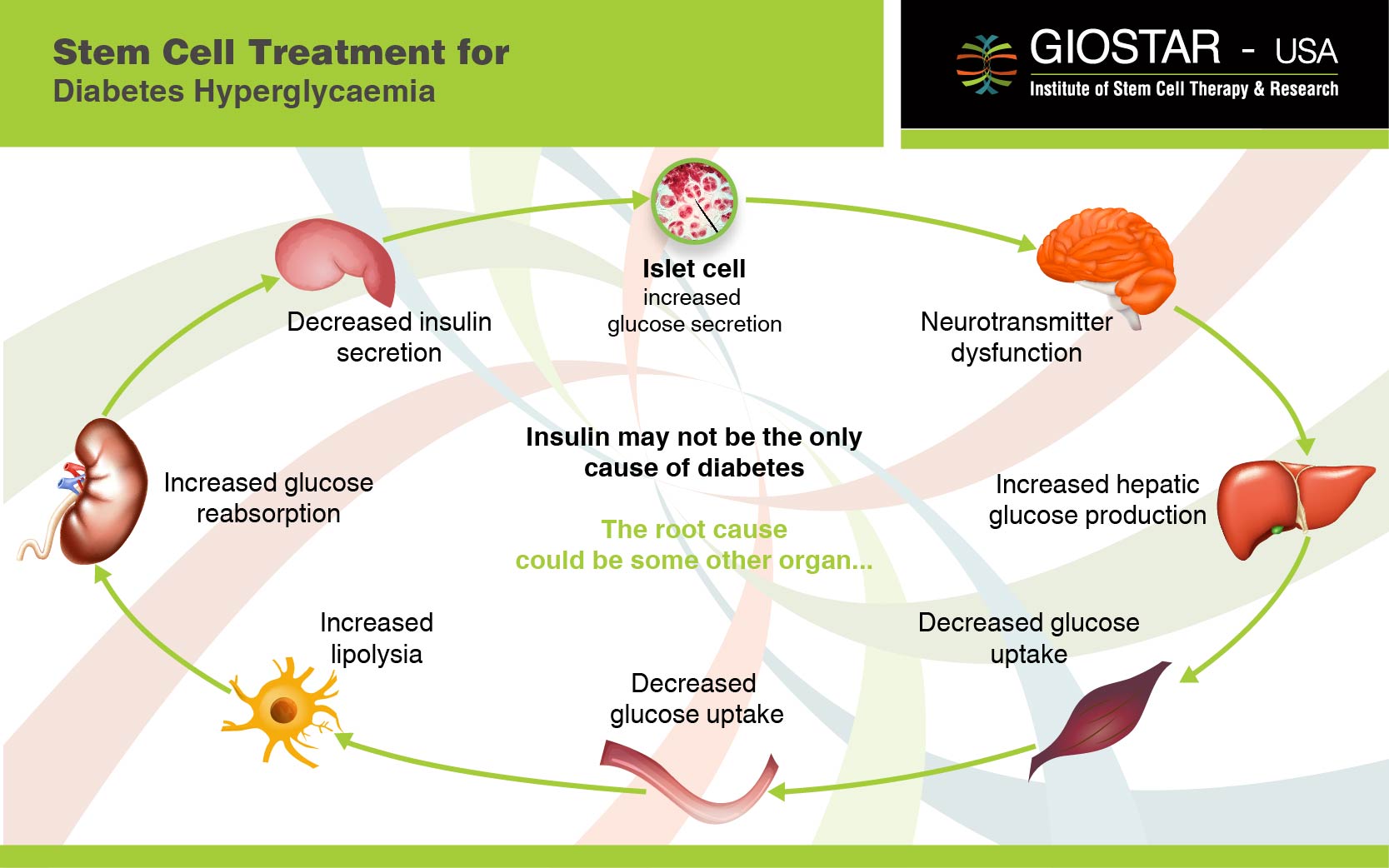
Stem cell therapy for T2D typically involves harvesting stem cells from the patient's own body (autologous) or, less commonly, from a donor (allogeneic). These cells, usually mesenchymal stem cells (MSCs), are then processed and reintroduced into the patient's body. The goal is to promote regeneration of damaged pancreatic beta cells (which produce insulin) and improve insulin sensitivity in other tissues, such as the liver and muscles.
The success of stem cell therapy depends on several factors, including the type of stem cells used, the method of delivery, the patient's overall health, and the stage of their diabetes. It is essential to manage expectations and realize this therapy isn't a guaranteed cure but rather a potentially powerful tool in managing the disease.
Success Rates: What Does the Research Say?
Determining a definitive "success rate" for stem cell therapy in T2D is complex due to variations in study design, patient populations, and outcome measures. However, several studies have shown promising results:
- Improved Glycemic Control: Many clinical trials have reported a reduction in HbA1c levels (a measure of average blood sugar over 2-3 months) following stem cell therapy. This indicates better overall blood sugar management.
- Reduced Insulin Dependence: Some patients have been able to reduce or even eliminate their need for insulin injections after stem cell therapy. This is a significant outcome as it decreases the burden of daily management.
- Enhanced Beta Cell Function: Studies have shown that stem cell therapy can improve the function of existing beta cells and potentially stimulate the regeneration of new beta cells. This contributes to increased insulin production.
- Decreased Complications: By improving glycemic control, stem cell therapy may help to reduce the risk of long-term diabetes complications, such as nerve damage (neuropathy), kidney disease (nephropathy), and eye damage (retinopathy).
It's important to note that the reported success rates vary considerably. Some studies report significant improvements in a large percentage of patients, while others show more modest effects. Long-term data on the durability of these effects is still being collected.
Real-world application: Stay updated on the latest clinical trials and research findings related to stem cell therapy for T2D. Resources like the National Institutes of Health (NIH) and medical journals are helpful.
Factors Influencing Success
Several factors can influence the success of stem cell therapy for T2D:
- Patient Selection: Ideal candidates for stem cell therapy are typically those with early-stage T2D who still have some residual beta cell function. Individuals with advanced diabetes and significant complications may experience less benefit.
- Type of Stem Cells: MSCs are the most commonly used stem cells for T2D therapy. The source and quality of these cells can affect the outcome.
- Delivery Method: Stem cells can be delivered intravenously (through a vein) or directly into the pancreas. The optimal delivery method is still being investigated.
- Lifestyle Modifications: Maintaining a healthy lifestyle, including a balanced diet and regular exercise, is crucial for maximizing the benefits of stem cell therapy.
- Post-Therapy Monitoring: Close monitoring of blood sugar levels, insulin requirements, and overall health is essential after stem cell therapy to assess its effectiveness and manage any potential complications.
Practical Considerations for Patients
If you're considering stem cell therapy for T2D, here are some practical steps you can take:
- Consult with Your Doctor: Discuss stem cell therapy with your endocrinologist or primary care physician. They can assess your suitability for the treatment and provide guidance.
- Research Reputable Clinics: Thoroughly research clinics that offer stem cell therapy. Look for clinics with experienced medical professionals, a track record of success, and ethical practices. Be wary of clinics making unrealistic promises or lacking proper credentials.
- Ask About Clinical Trials: Consider participating in a clinical trial. Clinical trials are designed to rigorously evaluate the safety and effectiveness of new treatments, and they can provide access to cutting-edge therapies.
- Understand the Risks and Benefits: Be aware of the potential risks and benefits of stem cell therapy. Discuss these with your doctor and the clinic providing the treatment. Risks can include infection, immune reactions, and unforeseen complications.
- Manage Expectations: Stem cell therapy is not a guaranteed cure for T2D. It's essential to have realistic expectations and understand that you may still need to manage your diabetes with lifestyle changes and medications.
- Prepare for Costs: Stem cell therapy can be expensive, and it may not be covered by insurance. Be sure to inquire about the costs and payment options before proceeding.
Actionable tip: Create a list of questions to ask potential clinics. Include questions about their experience, the type of stem cells used, the delivery method, the expected outcomes, and the potential risks and costs.
Integrating Stem Cell Therapy into Your Diabetes Management Plan
Stem cell therapy should be viewed as part of a comprehensive diabetes management plan that includes:
- Healthy Diet: Following a balanced diet low in processed foods, sugary drinks, and unhealthy fats is crucial for maintaining stable blood sugar levels. Work with a registered dietitian for personalized meal planning.
- Regular Exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, along with strength training exercises. Exercise improves insulin sensitivity and helps to control blood sugar.
- Medications: Continue taking your prescribed diabetes medications as directed by your doctor, even after stem cell therapy. Your doctor may adjust your medications based on your response to the treatment.
- Blood Sugar Monitoring: Regularly monitor your blood sugar levels to track your progress and make necessary adjustments to your diet, exercise, and medications.
- Stress Management: Practice stress-reducing techniques such as yoga, meditation, or deep breathing exercises. Stress can affect blood sugar levels and overall health.
Practical advice: Keep a detailed food journal to track your carbohydrate intake and its impact on your blood sugar levels. This can help you make informed dietary choices and optimize your glycemic control.
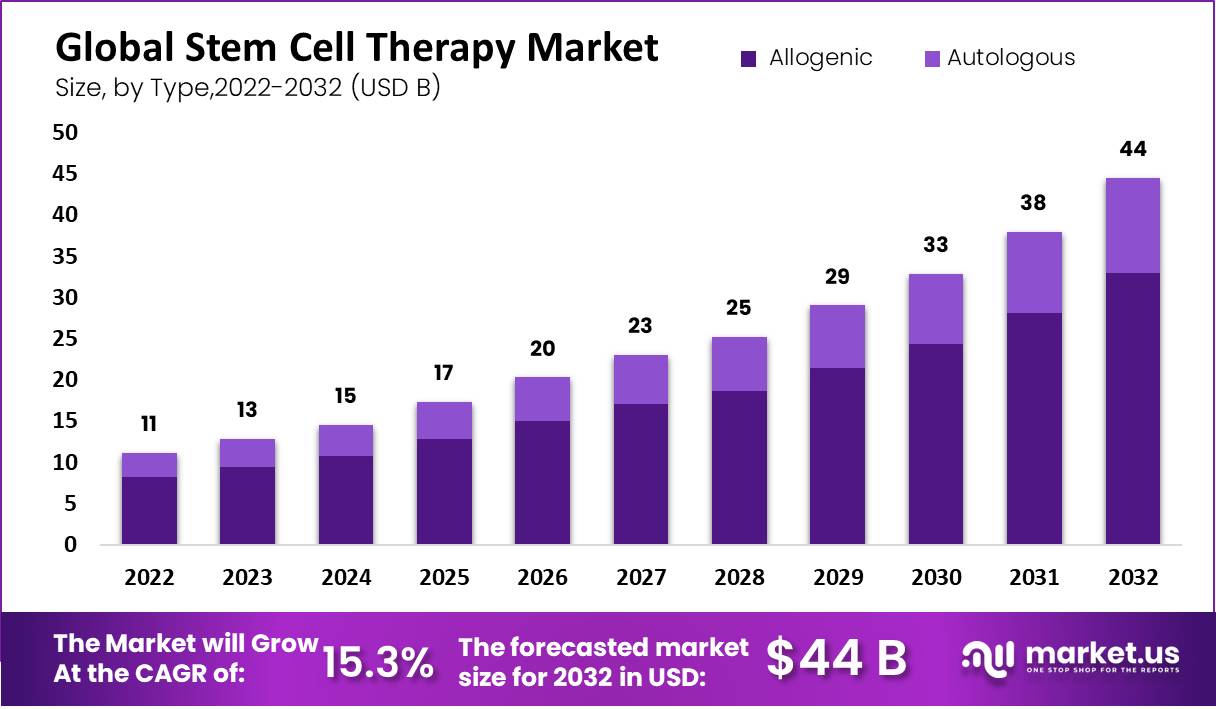
Looking Ahead: The Future of Stem Cell Therapy for Type 2 Diabetes
Research in stem cell therapy for T2D is ongoing, and scientists are working to improve the efficacy and safety of these treatments. Future advancements may include:
- Developing More Effective Stem Cell Types: Researchers are exploring different types of stem cells and methods for enhancing their ability to regenerate beta cells and improve insulin sensitivity.
- Improving Delivery Methods: New delivery methods are being developed to ensure that stem cells reach the pancreas and other target tissues effectively.
- Personalized Stem Cell Therapy: As we learn more about the individual factors that influence the success of stem cell therapy, treatments may become more personalized to each patient's specific needs.
Stay informed: Follow reputable medical news sources and organizations dedicated to diabetes research to stay updated on the latest advancements in stem cell therapy.
Checklist/Guideline for Considering Stem Cell Therapy
Before Considering Stem Cell Therapy:During Stem Cell Therapy:
- Consult with your endocrinologist or primary care physician.
- Research reputable clinics offering stem cell therapy.
- Understand the potential risks, benefits, and costs.
- Manage your expectations and realize it's not a guaranteed cure.
- Consider participating in a clinical trial.
After Stem Cell Therapy:
- Follow your doctor's instructions carefully.
- Maintain a healthy lifestyle, including a balanced diet and regular exercise.
- Monitor your blood sugar levels regularly.
- Continue taking your prescribed diabetes medications as directed.
- Attend follow-up appointments with your doctor.
- Be patient and allow time for the treatment to take effect.
- Report any unusual symptoms or side effects to your doctor.
Disclaimer: This information is for educational purposes only and should not be considered medical advice. Always consult with a qualified healthcare professional before making any decisions about your health or treatment.