Okay, okay, gather 'round, friends! Let's talk about something super exciting... Primary Assessments! I know, I know, sounds about as thrilling as watching paint dry, but trust me, it's way more important than picking the right shade of beige for your living room. Think of it as the superhero origin story for saving someone's life. Without it, you're basically stumbling around in the dark, hoping for a miracle. And miracles are great, but a solid primary assessment is way more reliable.
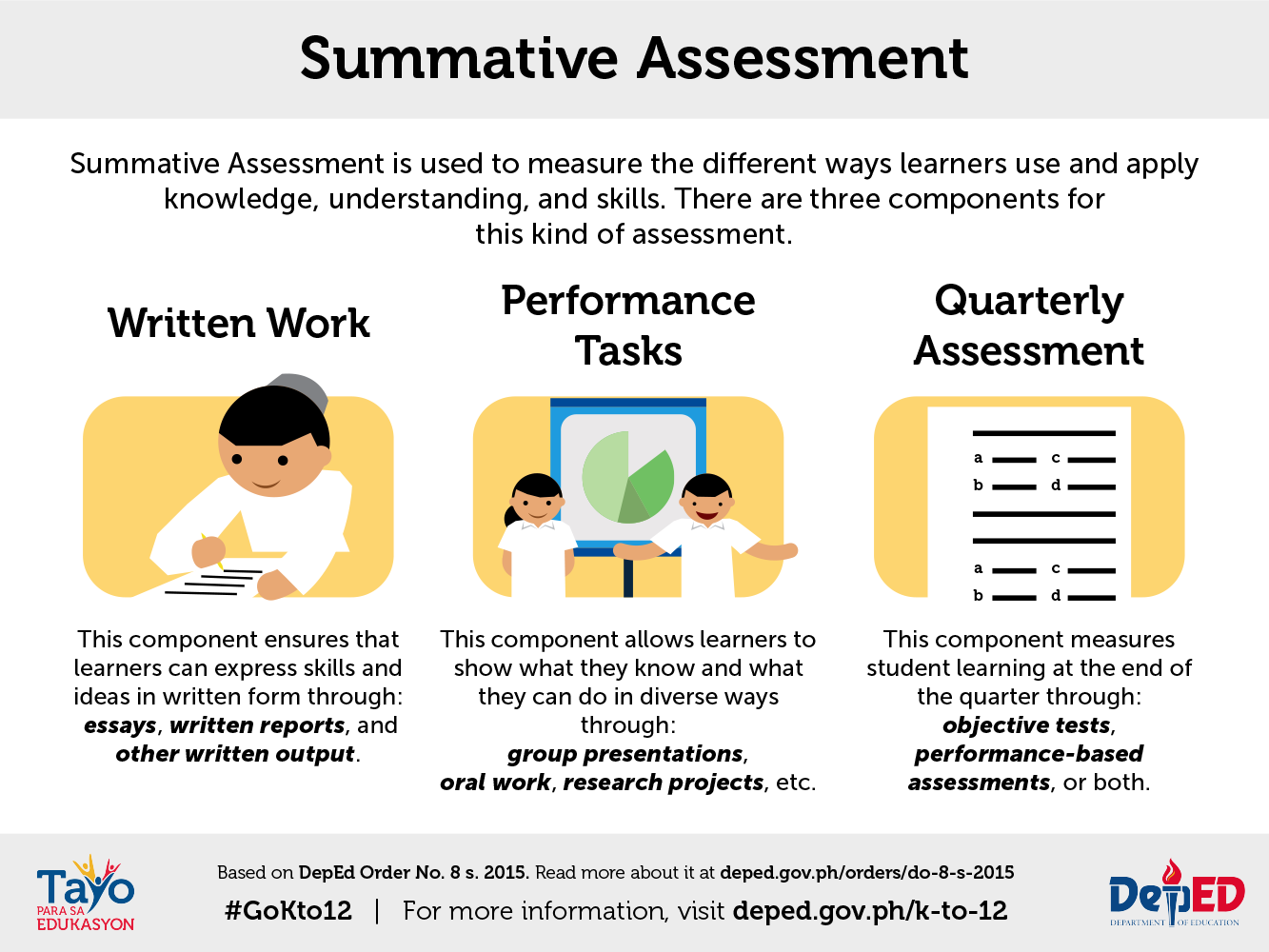
What in the World is a Primary Assessment?
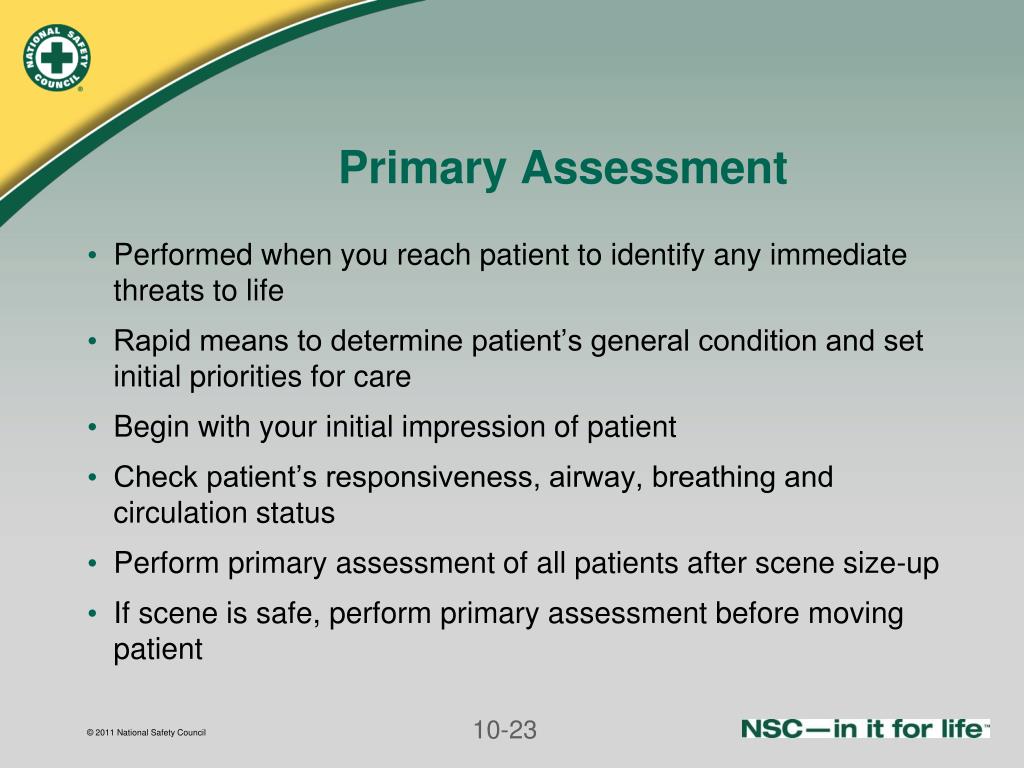
Imagine this: you walk into a scene, maybe someone tripped over a rogue garden gnome (it happens!), or perhaps they're just dramatically slumped on a park bench (we've all been there). The primary assessment is your quick and dirty way of figuring out if they're about to have a really, REALLY bad day. It's like speed dating, but for life-saving. You need to quickly size up the situation and decide if this person needs immediate intervention. We're talking about life-or-death stuff, folks. No pressure.
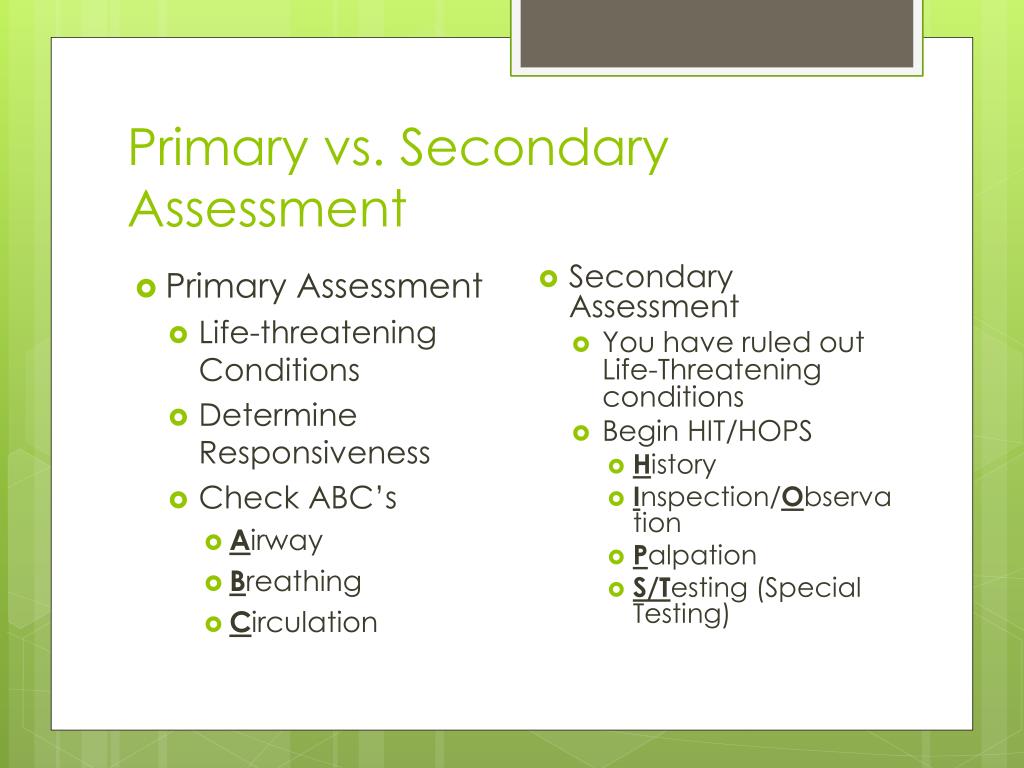
It's essentially a rapid-fire survey of the most vital functions of the human body. Think of it as the body's VIP list: only the most important guests (systems) get immediate attention.
The Goal: Not Just Playing Doctor, But Being a Lifesaver!
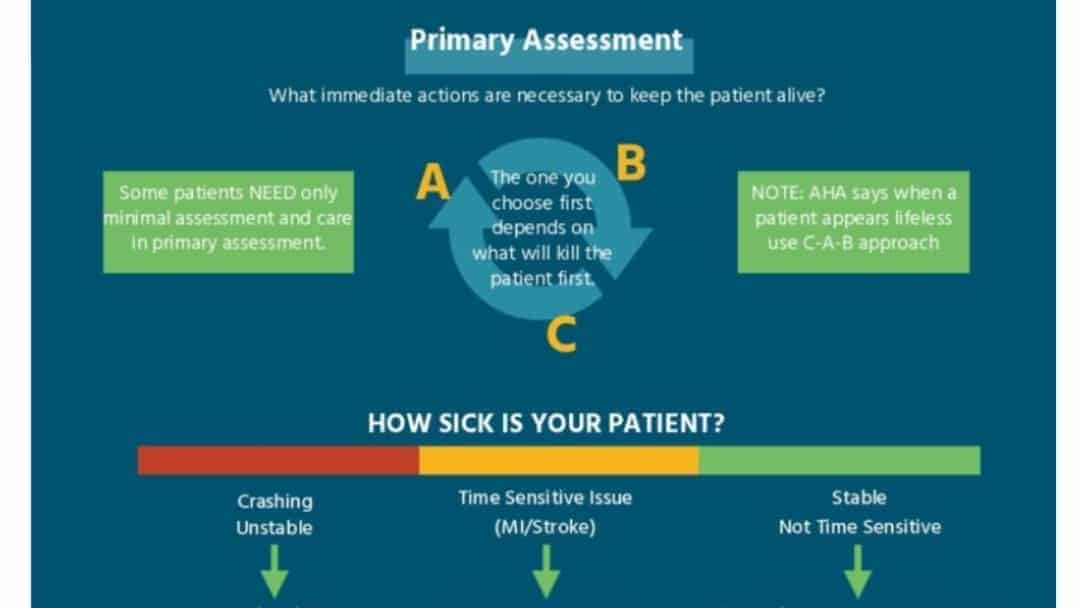
So, what's the ultimate goal? Drumroll please... To identify and treat any immediate life threats! Boom! Mic drop! Okay, maybe not a literal mic drop, those are expensive. But you get the idea. We're not aiming for a detailed medical history here. We're not trying to diagnose their childhood allergies. We're trying to make sure they're not about to stop breathing or bleed out on our watch.
Think of it like this: you're a triage nurse at the ER of Life. You don't have time for chit-chat; you need to figure out who needs your help right now. It's all about prioritization, baby!
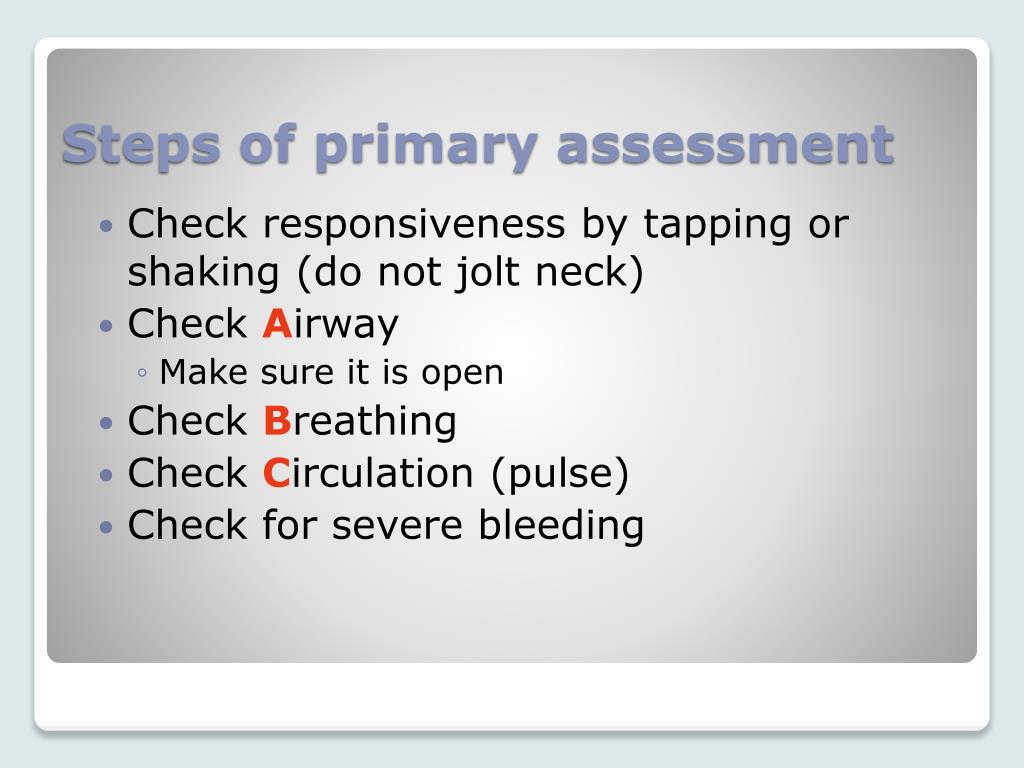
The ABCs (and sometimes Ds & Es) of Awesomeness
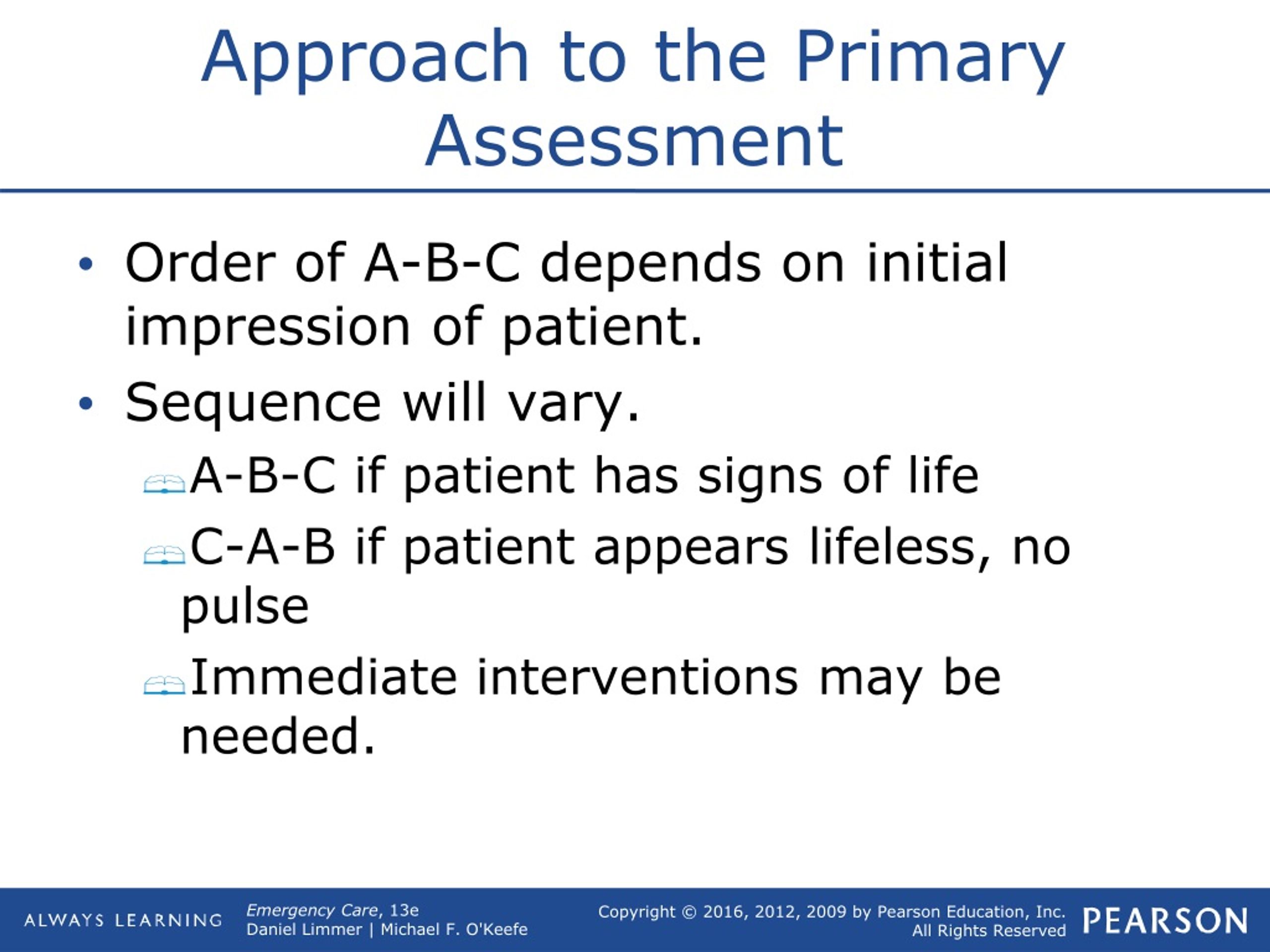
Now, how do we achieve this goal? Well, buckle up, buttercup, because we're about to dive into the alphabet soup of life-saving goodness. I'm talking about the ABCs of primary assessment:
A is for Airway: The Road to Life
First up, Airway! This is where we ask ourselves: Is the airway open? Can the person breathe? Imagine trying to drink a milkshake through a straw that's been crumpled. Not fun, right? Same goes for breathing. If the airway is blocked by, say, their tongue (it happens when you're unconscious!), or some rogue chewing gum, we need to fix it immediately. We might use maneuvers like the head-tilt/chin-lift or the jaw-thrust (if you suspect a neck injury). Think of yourself as a skilled plumber, unclogging the pipes of life!
- Is the airway patent? (That's fancy medical talk for "is it open?")
- Look, listen, and feel for breathing. (Look for chest rise, listen for breath sounds, and feel for air movement.)
- If blocked, open it! (Head-tilt/chin-lift, jaw-thrust, suctioning if needed.)
B is for Breathing: The Air We Share
Next, we have Breathing! Okay, so the airway is open, but are they actually breathing effectively? Are they breathing fast, slow, deep, shallow, like a goldfish out of water? We're looking for signs of respiratory distress. Things like rapid breathing, shallow breaths, using accessory muscles (those neck muscles get a workout!), or just generally looking like they're about to pass out from lack of oxygen. If they're not breathing adequately, we might need to assist them with a bag-valve-mask (BVM) or even consider advanced airway techniques. Don't worry, you'll learn all that in your CPR/First Aid class!
- What's the breathing rate? (Normal is usually 12-20 breaths per minute for adults.)
- Is the breathing effort normal? (Are they struggling to breathe?)
- Is there good chest rise? (Is the chest expanding and contracting with each breath?)
C is for Circulation: The Blood Must Flow!
And now, for the grand finale of the ABCs: Circulation! This is all about the blood, baby! Is the heart pumping? Is the blood flowing? Are they bleeding like they just starred in a Quentin Tarantino film? We need to check for a pulse (carotid is usually the easiest in an unresponsive patient), assess skin color and temperature (pale, cool, and clammy is not a good sign!), and control any major bleeding. Direct pressure is your best friend here. Think of yourself as a blood-stopping superhero! If there's no pulse, well, that's when we start CPR. But hopefully, we can avoid that.
- Check for a pulse. (Carotid is best in unresponsive patients.)
- Assess skin color, temperature, and condition. (Pale, cool, clammy = bad news.)
- Control any major bleeding. (Direct pressure is your superpower.)
Sometimes There's a D and E Too! (Just to Keep Things Interesting)
Now, depending on the situation and your level of training, you might also include D and E in your primary assessment.
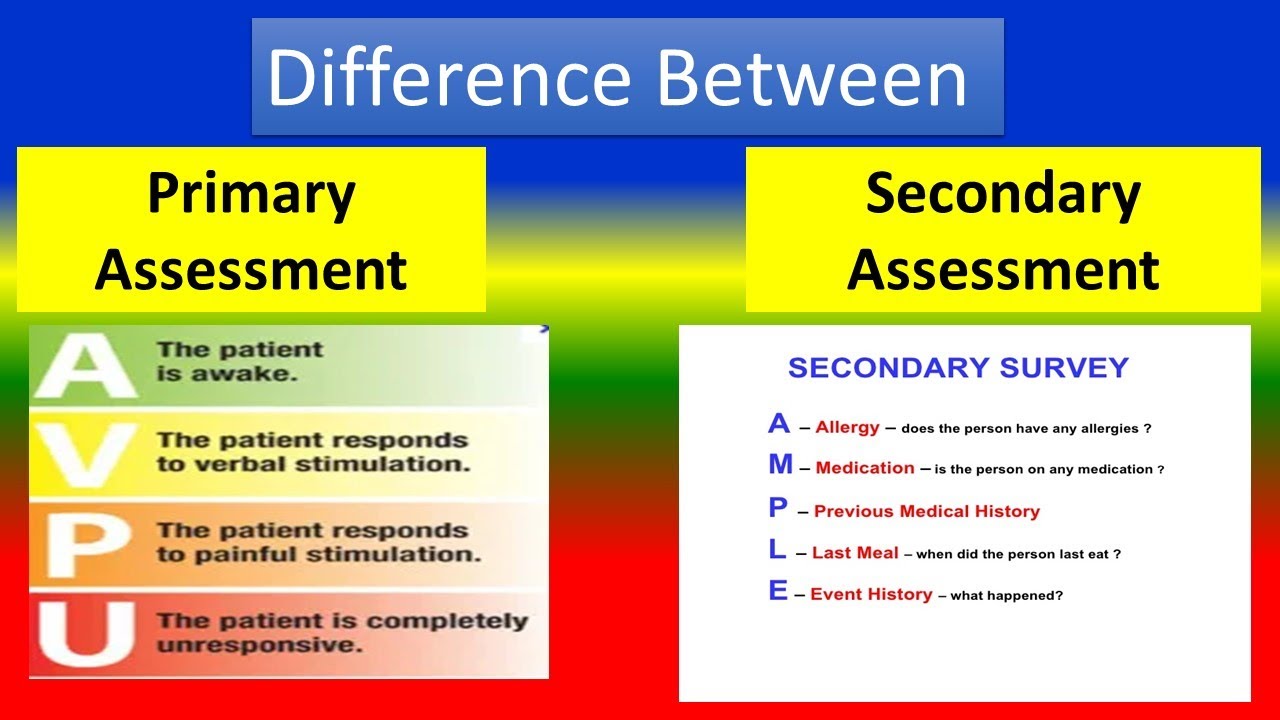
D is for Disability: Brain Power Check!
D stands for Disability, which basically means assessing the person's level of consciousness. Are they awake, alert, and oriented? Or are they completely unresponsive? We might use a simple scale like the AVPU scale (Alert, Verbal, Painful, Unresponsive) to quickly gauge their neurological status. It's a quick check to see if their brain is working (or at least attempting to work).
E is for Exposure: Stripping Away the Secrets (Carefully!)
Finally, we have E for Exposure. This means exposing the patient (carefully and respectfully, of course!) to look for any injuries that might be hidden under their clothing. We want to see if there are any obvious signs of trauma, like deformities, bruising, or lacerations. Remember to keep the patient warm to prevent hypothermia! Think of yourself as a detective, searching for clues to solve the medical mystery.
Why Bother? The Importance of Speed and Accuracy
So, why is all this so important? Because every second counts! A delay in identifying and treating a life-threatening condition can have devastating consequences. Imagine being stuck in traffic during rush hour, every minute feels like an eternity, right? Now imagine that traffic jam is inside someone's body, preventing oxygen from reaching their brain. Not a fun scenario.
A well-executed primary assessment allows you to quickly prioritize the patient's needs and provide the appropriate interventions. It's the difference between a calm, organized response and a chaotic scramble. It's the key to turning a potential tragedy into a success story. And who doesn't love a good success story?
In Conclusion: Be a Primary Assessment Pro!
The goal of the primary assessment is simple: identify and treat immediate life threats. By following the ABCs (and sometimes Ds and Es) and acting quickly and decisively, you can make a real difference in someone's life. So go out there, be confident, be prepared, and be a primary assessment pro! You might just save a life. And that, my friends, is way more rewarding than finding the perfect shade of beige.
.jpg)







.jpg)