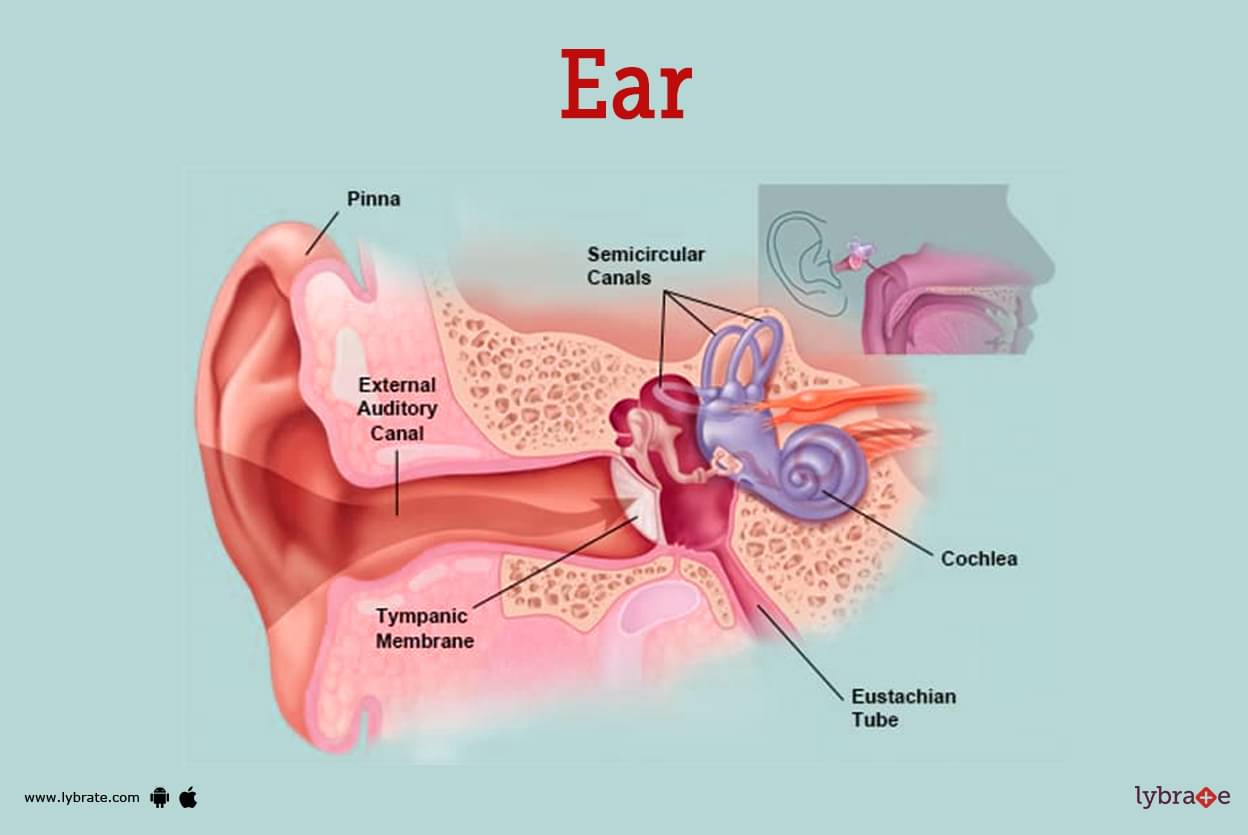
The eardrum, or tympanic membrane, is a vital component of the auditory system, responsible for converting sound waves into mechanical vibrations that are then transmitted to the inner ear. While we often understand its function, visualizing the eardrum's appearance on camera, particularly during otoscopic examination, reveals a fascinating interplay of anatomy, diagnostic capabilities, and technological advancements. What we see is not merely a flat surface, but a landscape of subtle indicators reflecting health and potential pathology.
Causes of Variations in Eardrum Appearance
The appearance of the eardrum on camera can vary significantly depending on several factors. These can be broadly categorized into anatomical variations, pathological conditions, and technical considerations related to the imaging process itself. Anatomical variations, though normal, contribute to a range of observed appearances.
Anatomical Factors
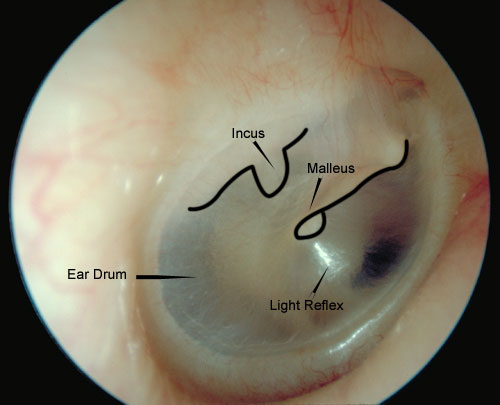
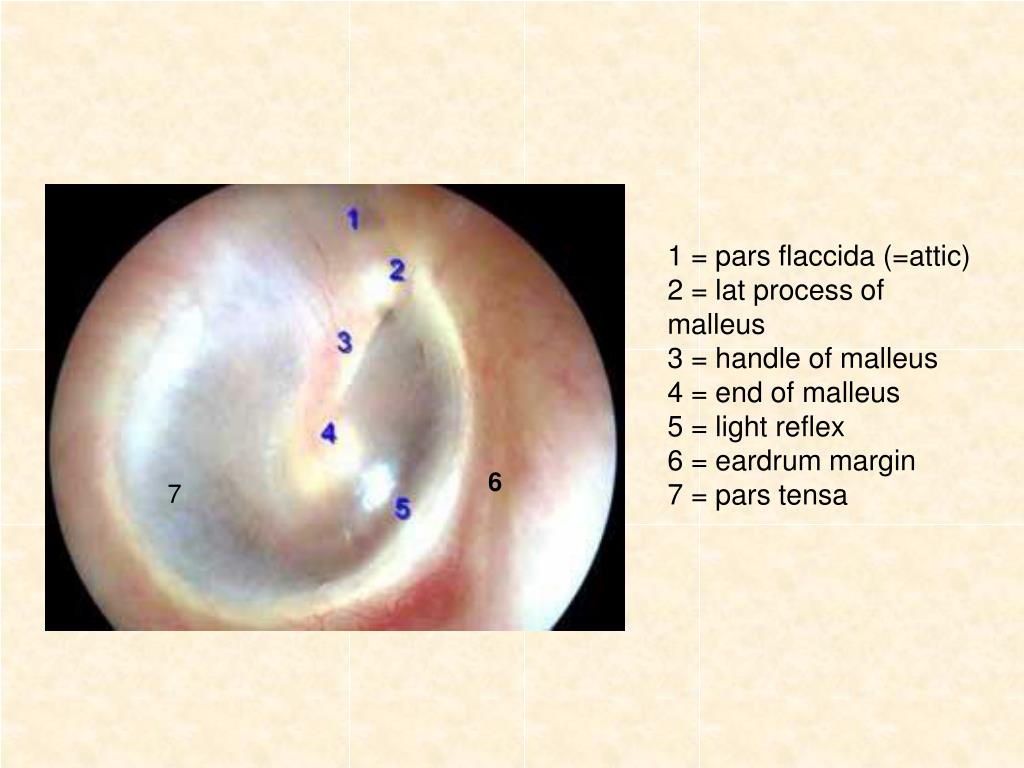
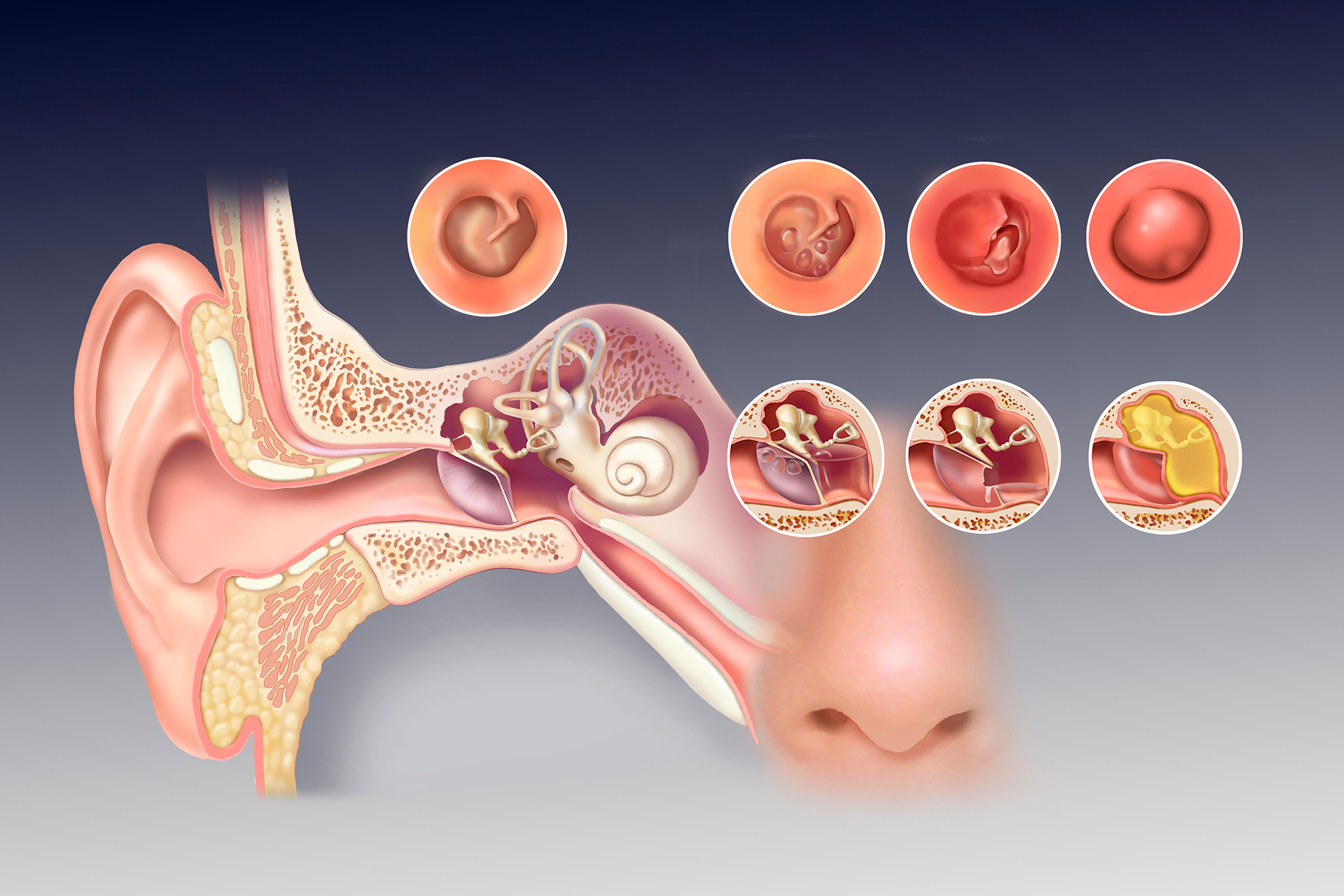
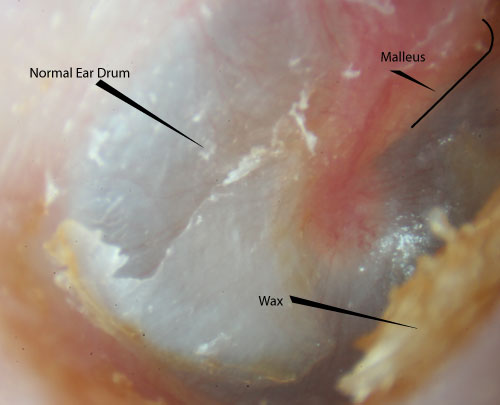
Naturally occurring differences in the eardrum's size, shape, and thickness contribute to variations. For example, the cone of light, a triangular reflection of the otoscope's light, may appear sharper or more diffuse depending on the eardrum's curvature. Furthermore, the presence of prominent anatomical landmarks like the malleus (one of the ossicles, or small bones, of the middle ear) can alter the visible surface. Its prominence or obscuration can hint at the presence or absence of fluid in the middle ear. The pars tensa, the largest and tautest part of the eardrum, and the pars flaccida, a smaller, more pliable region, also exhibit differing light reflectivity and transparency.
Pathological Conditions
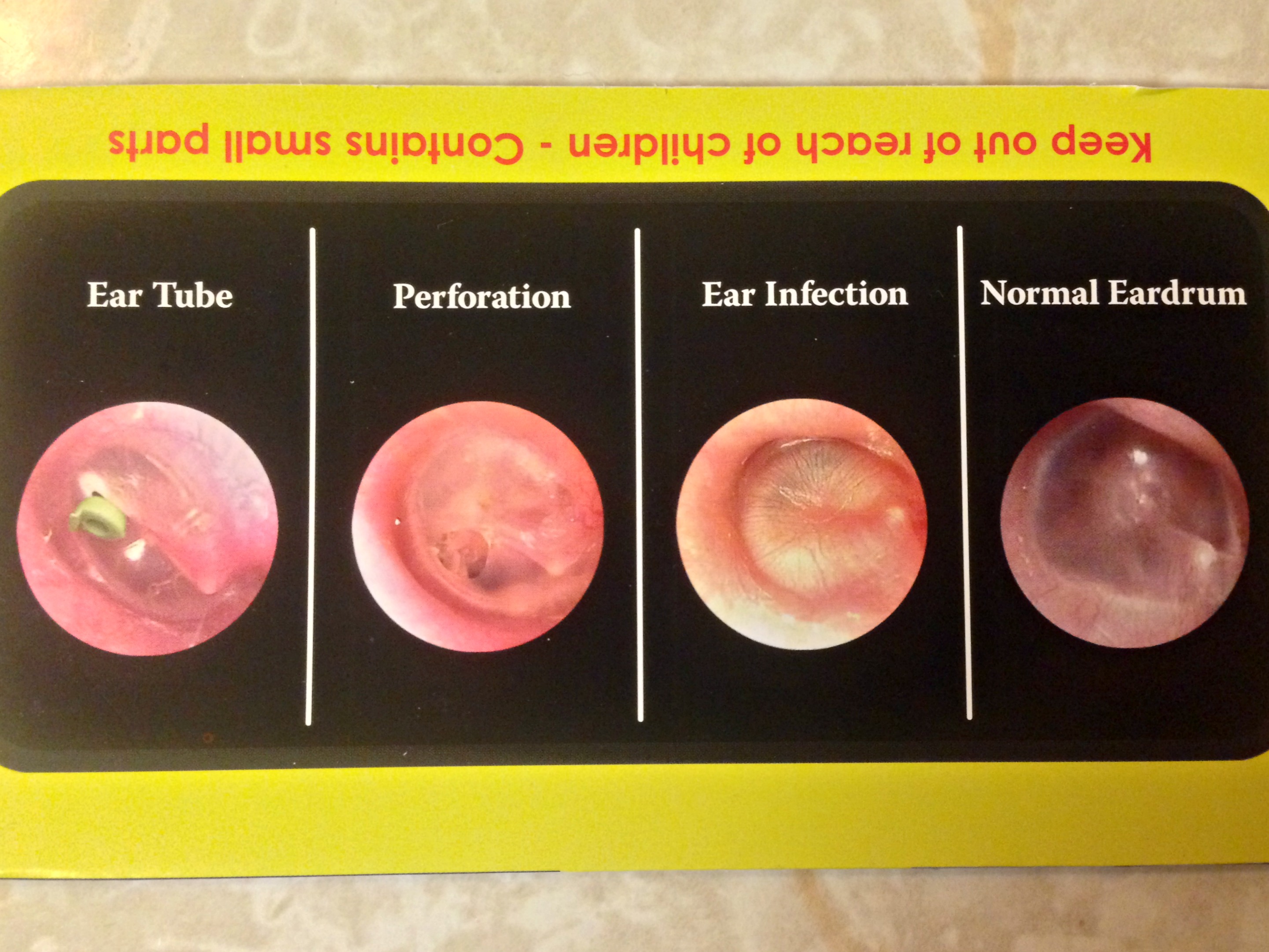
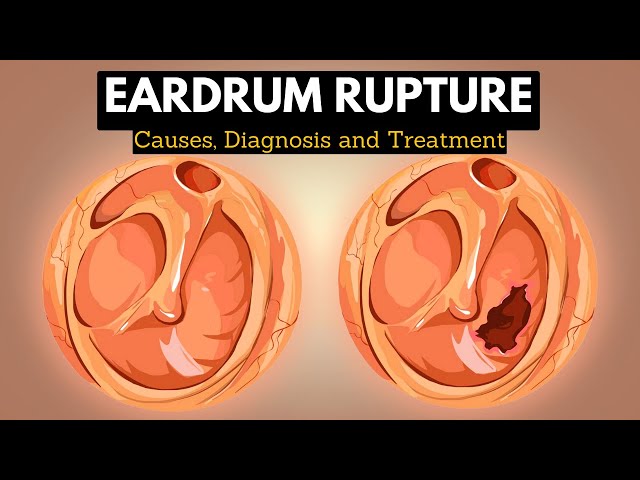
A wide array of pathological conditions can dramatically alter the eardrum's appearance. Infections, trauma, and chronic diseases are prime examples. Otitis media, a common ear infection, often presents with a red, bulging eardrum, potentially accompanied by pus or fluid visible behind the membrane. A perforated eardrum, caused by trauma or infection, will appear as a hole or tear. According to the National Institute on Deafness and Other Communication Disorders (NIDCD), otitis media is one of the most common reasons children visit a doctor, highlighting the prevalence and importance of recognizing its visual markers.
Chronic conditions, such as tympanosclerosis, can cause the eardrum to become thickened and scarred, leading to opaque white patches. Cholesteatoma, a benign but destructive growth in the middle ear, can manifest as a pearly white mass behind the eardrum, or even erode through the membrane. The location, color, and texture of any observed abnormalities are crucial diagnostic clues.
Technical Factors
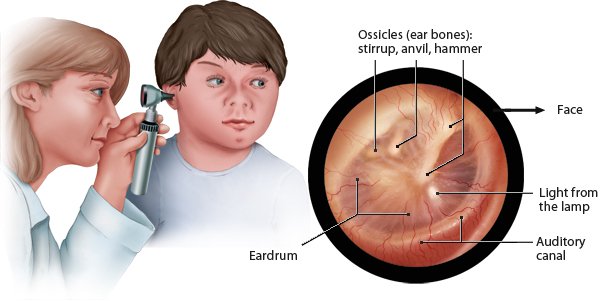
The quality of the imaging equipment significantly impacts the visible appearance of the eardrum. Otoscopes with poor light sources or inadequate magnification can distort the image, making it difficult to discern subtle details. Endoscopes, which offer superior visualization due to their ability to navigate the ear canal more effectively, provide clearer and more detailed images compared to traditional otoscopes. The angle of the camera, the lighting conditions, and the presence of earwax (cerumen) can also influence the image quality. It is essential to clean the ear canal before examination to ensure optimal visualization. The resolution of the camera and the monitor also play a key role in the level of detail that can be observed.
Effects of Accurate Eardrum Visualization
Accurate visualization of the eardrum has profound effects on diagnosis, treatment, and patient outcomes. The ability to clearly see the eardrum allows healthcare professionals to:
Improved Diagnosis
Clear imaging enables a more accurate and timely diagnosis of ear conditions. This is particularly crucial in pediatric cases, where young children may struggle to articulate their symptoms. Early detection of infections, perforations, or other abnormalities allows for prompt intervention, preventing potential complications like hearing loss or speech delays. Tele-otoscopy, the practice of remotely examining the eardrum using specialized cameras and telecommunication technology, expands access to specialist care in underserved areas. Remote diagnosis, facilitated by high-quality imaging, can bridge geographical barriers and improve patient outcomes.
Targeted Treatment
Accurate diagnosis informs targeted treatment strategies. For example, if the eardrum appears red and bulging, indicating an acute infection, antibiotics may be prescribed. If a perforation is present, the size and location of the hole will influence the decision between observation, antibiotic ear drops, or surgical repair. In cases of cholesteatoma, early detection and surgical removal are essential to prevent further damage to the middle ear and surrounding structures. Precise visualization guides surgical planning and execution, leading to better outcomes.
Monitoring Treatment Progress
Serial imaging of the eardrum allows healthcare professionals to monitor the progress of treatment and assess the effectiveness of interventions. For instance, after starting antibiotics for an ear infection, subsequent otoscopic examinations can reveal whether the redness and bulging are resolving. Similarly, after surgical repair of a perforated eardrum, follow-up imaging can confirm the successful closure of the perforation. Consistent visual documentation provides objective evidence of treatment efficacy and allows for adjustments to the treatment plan as needed.
Implications of Advancements in Eardrum Imaging
Advancements in eardrum imaging technology are continuously expanding the diagnostic and therapeutic capabilities of otolaryngology. These advancements carry significant implications for healthcare delivery and patient care.
Enhanced Diagnostic Accuracy
High-resolution cameras, endoscopes, and optical coherence tomography (OCT) are revolutionizing eardrum imaging. OCT, in particular, provides non-invasive, cross-sectional images of the eardrum and middle ear structures, allowing for the detection of subtle abnormalities that may not be visible with traditional otoscopy. These advanced imaging techniques enhance diagnostic accuracy, reduce the need for invasive procedures, and improve patient outcomes. For instance, OCT can differentiate between fluid and thickened mucosa in the middle ear, guiding treatment decisions in cases of chronic otitis media.
Improved Patient Education and Engagement
Sharing images of the eardrum with patients can enhance their understanding of their condition and promote active participation in their care. Visual evidence of the problem can be more impactful than verbal explanations alone. Patients are more likely to adhere to treatment plans when they understand the underlying pathology and the rationale for the prescribed interventions. Showing a patient an image of their perforated eardrum, for example, can underscore the importance of protecting the ear from water and infection.
Artificial Intelligence and Automated Diagnosis
The application of artificial intelligence (AI) to eardrum imaging holds immense promise for automated diagnosis and improved efficiency. AI algorithms can be trained to recognize patterns and features in eardrum images that are indicative of specific diseases. This technology has the potential to assist healthcare professionals in making accurate and timely diagnoses, particularly in resource-limited settings where specialist expertise may be scarce. However, the reliability and accuracy of AI-based diagnostic tools must be rigorously validated before widespread implementation.
Looking at an eardrum on camera is far more than just a visual exercise; it is a window into the health of the auditory system. Understanding the subtle nuances of what we see - the variations in color, shape, and landmarks - empowers healthcare professionals to make informed decisions that ultimately impact patient well-being. As imaging technology continues to evolve, so too will our ability to diagnose and treat ear disorders with greater precision and efficacy.