Okay, so picture this: I'm at a concert, right? Finally seeing my favorite band. But after three hours of jumping, dancing (or, let's be real, awkward swaying), and generally being vertically challenged in a crowd, my legs felt like they were filled with cement. Not the cool, smooth kind, but the lumpy, half-dried stuff. It wasn't just tired, it was heavy. That, my friends, was my first real introduction to the delightful sensation of blood pooling in my legs.
Ever felt that? That kind of lead-weight feeling? It’s surprisingly common, and it’s worth understanding what’s going on down there. Because while sometimes it's just a minor inconvenience, other times it can signal something you need to, you know, *actually* pay attention to.
What Exactly Is Blood Pooling?
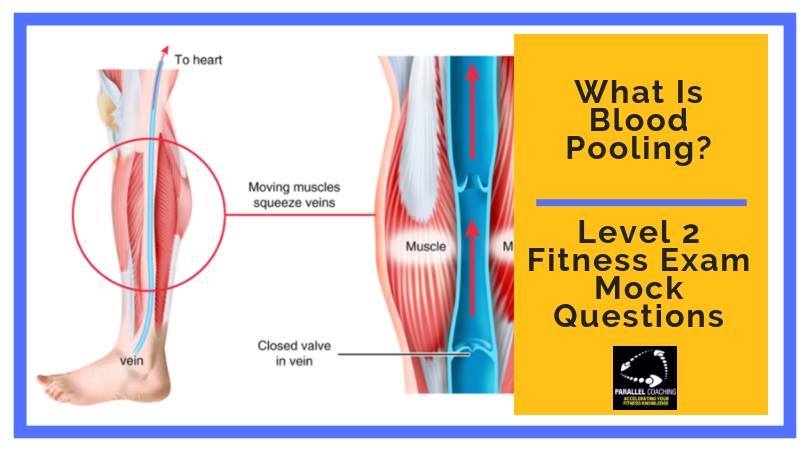
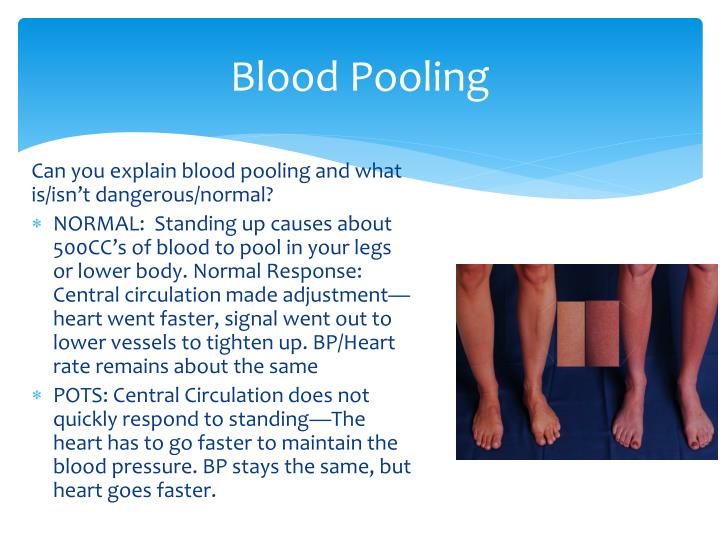
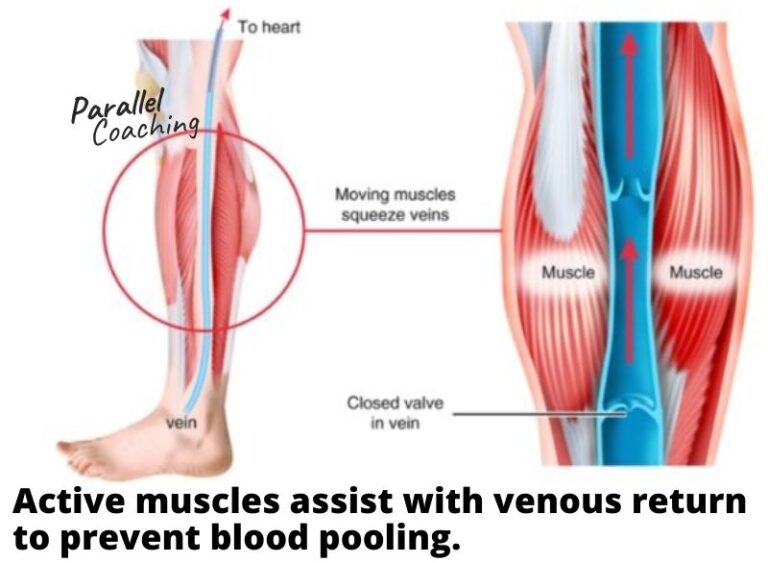
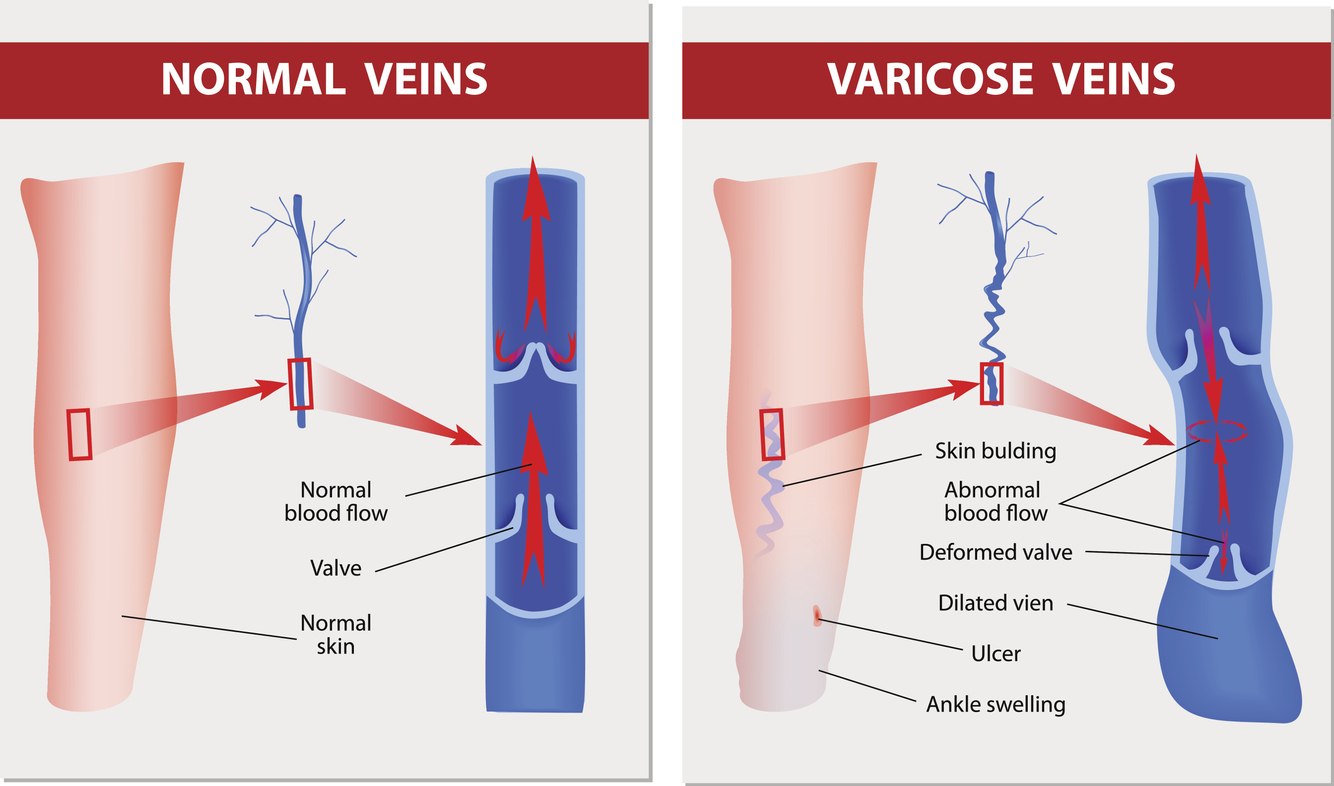
Alright, let’s get a little science-y, but I promise to keep it brief. Basically, your circulatory system is supposed to be a smooth, two-way street. Arteries pump blood away from your heart, delivering oxygen and nutrients to all your tissues. Veins bring the blood back to your heart to get re-oxygenated. So far, so good, right?
The problem is gravity. That sneaky little force is constantly trying to pull everything down, including your blood. When you're standing or sitting for long periods, especially without moving much, it becomes harder for your veins to efficiently pump blood back up to your heart. This is where the "pooling" happens: blood starts to accumulate in your lower extremities, because, well, that's where gravity likes it best.
(Think of it like trying to pump water uphill with a weak pump. Some water gets there, but a lot just settles back down. That’s your veins when they’re struggling!)
The Many (Not-So-Fun) Feelings of Pooled Blood
Now, what does all this pooling actually *feel* like? It's not always the same for everyone, but here are some of the common sensations:
- Heaviness: This is the big one. Your legs might feel incredibly heavy, like you're dragging anchors. Imagine trying to walk with weights strapped to your ankles – that's the ballpark.
- Aching: A dull, throbbing ache is another frequent complaint. It’s not a sharp pain, but more of a constant, nagging discomfort. (Like the feeling you get after a really intense workout, but without the workout part...which is arguably worse).
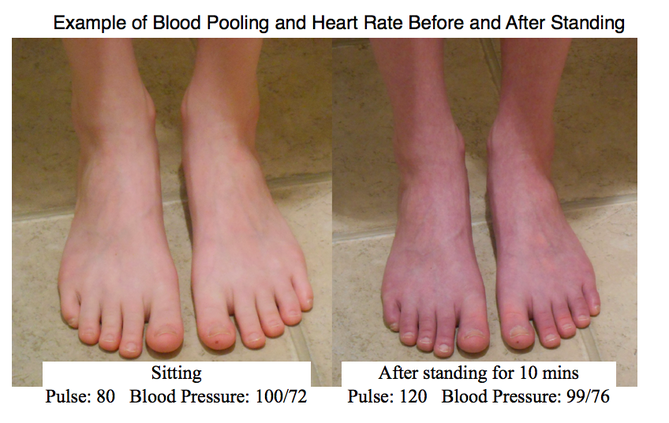
- Swelling (Edema): This is when you start to notice visible puffiness, especially in your ankles and feet. Press your finger into the swollen area – if it leaves a temporary indentation (pitting edema), that’s a pretty good sign of fluid retention, which can be caused by blood pooling.
- Tingling or Numbness: Sometimes, the pressure from the pooled blood can affect the nerves in your legs and feet, leading to a tingling or numb sensation. This is similar to the feeling you get when your foot "falls asleep," but it might be more persistent.
- Throbbing: You might feel a distinct throbbing sensation in your legs, especially in your calves or ankles. This is likely due to the increased pressure in your veins.
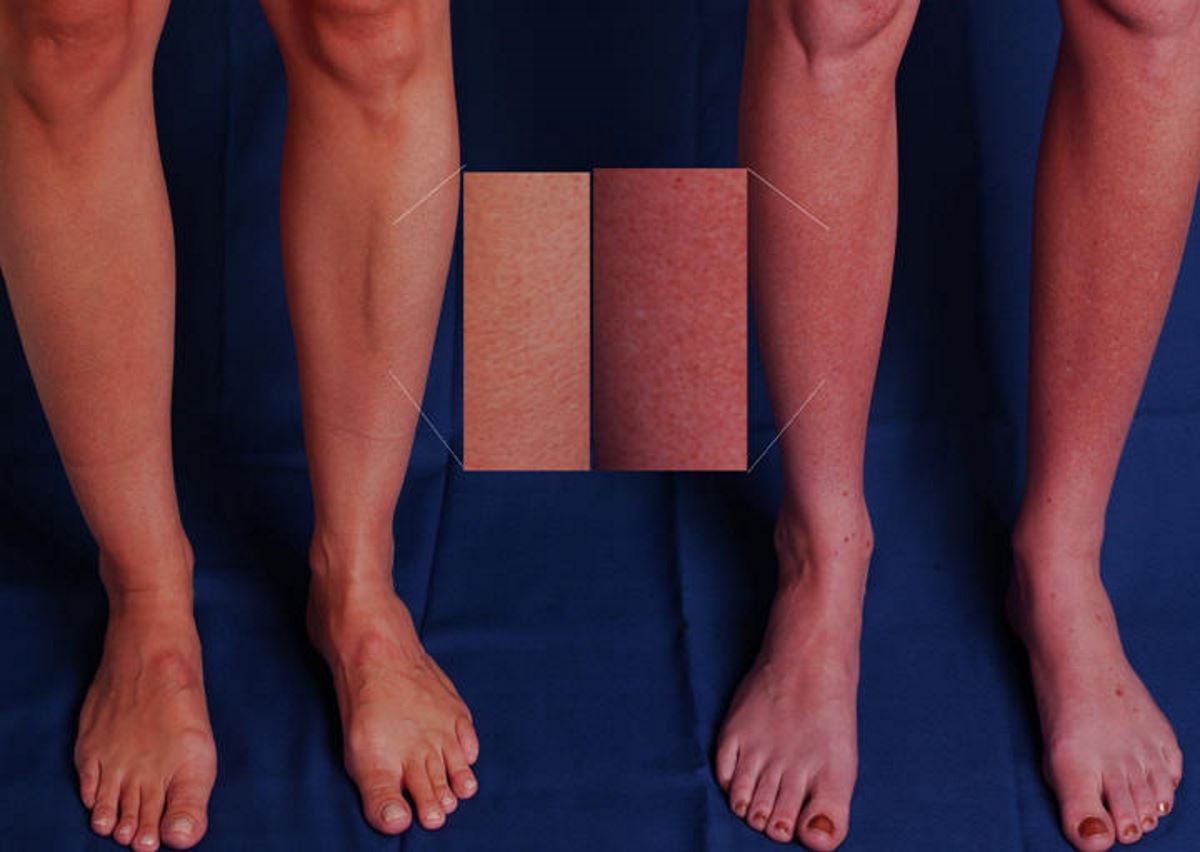
- Skin Discoloration: In more severe cases, prolonged blood pooling can lead to skin discoloration, often a bluish or reddish hue. This indicates that the tissues aren't getting enough oxygen. (Okay, this is where you *definitely* want to talk to a doctor.)
- Itchiness: Sometimes, swelling can cause the skin to stretch and become itchy. Resisting the urge to scratch is tough, but scratching can further irritate the skin and even lead to infection.
- Fatigue: Your legs just feel... tired. Like, bone-deep tired. Even a short walk can leave you feeling exhausted.
Notice how I said "sensations"? Because it's not always just one thing. Sometimes it's a delightful cocktail of heaviness, aching, and tingling, all rolled into one lovely package. (Said no one ever, of course).
Why Is This Happening to Me? (Possible Causes)
Okay, so you're feeling the leg-cement syndrome. What's causing it? Here are some of the usual suspects:
- Prolonged Standing or Sitting: This is the most common culprit. Think long flights, road trips, or jobs that require you to be on your feet all day. Your veins just get tired of fighting gravity.
- Pregnancy: Pregnancy puts extra pressure on the veins in your legs, making it harder for them to pump blood back to your heart. Hormonal changes during pregnancy can also relax vein walls, further contributing to pooling.
- Obesity: Excess weight puts additional strain on your circulatory system, making it more difficult for your veins to function efficiently.
- Age: As we age, our veins tend to lose elasticity, making them less effective at pumping blood. Sorry, but it’s true.
- Varicose Veins: These are enlarged, twisted veins that can develop when valves in the veins become weak or damaged. They hinder proper blood flow and contribute to pooling.
- Chronic Venous Insufficiency (CVI): This is a more serious condition in which the valves in your leg veins don't work properly, causing blood to pool. It can lead to more severe symptoms like skin ulcers.
- Blood Clots (Deep Vein Thrombosis - DVT): A blood clot in a deep vein can block blood flow and cause significant pooling, swelling, and pain. This is a medical emergency and requires immediate attention.
- Certain Medications: Some medications, like birth control pills and hormone replacement therapy, can increase the risk of blood clots and venous insufficiency.
- Heart Conditions: Certain heart conditions can affect blood flow and contribute to blood pooling in the legs.
So, yeah, the causes range from "oops, I sat too long" to "oh dear, this needs a doctor, like, yesterday."
What Can I Do About It? (Relief and Prevention)
Alright, let's talk solutions. Here are some things you can do to alleviate the symptoms of blood pooling and prevent it from happening in the first place:
- Elevate Your Legs: This is the simplest and often most effective remedy. Prop your legs up on pillows or a footrest whenever possible, especially when you're sitting or lying down. Aim to get your feet above your heart.
- Compression Stockings: These special stockings provide gentle pressure to your legs, helping to support your veins and improve blood flow. They come in different levels of compression, so talk to your doctor or a pharmacist to find the right ones for you. (They're not exactly high fashion, but trust me, your legs will thank you.)
- Move Around: Avoid sitting or standing for long periods without taking breaks to move around. Even a few minutes of walking or stretching can make a big difference. If you have a desk job, try setting a timer to remind you to get up and move every hour.
- Exercise Regularly: Regular exercise, especially activities that work your calf muscles (like walking, running, or swimming), can improve circulation and strengthen your veins.
- Maintain a Healthy Weight: Losing weight if you're overweight or obese can reduce the strain on your circulatory system.
- Stay Hydrated: Dehydration can thicken your blood, making it harder for it to flow. Drink plenty of water throughout the day.
- Avoid Tight Clothing: Restrictive clothing, especially around your waist and legs, can impede blood flow. Opt for looser, more comfortable clothing.
- Reduce Salt Intake: Too much salt can lead to fluid retention, which can worsen blood pooling.
- Take Breaks During Long Trips: If you're traveling by plane or car, get up and walk around every hour or two. If you can't get up, do some ankle pumps and leg stretches in your seat.
- Consider Vein Treatments: If you have varicose veins or chronic venous insufficiency, your doctor may recommend treatments like sclerotherapy (injecting a solution into the veins to close them off) or laser ablation (using heat to close the veins).
Think of these as little acts of kindness for your legs. They’ll appreciate it!
When to See a Doctor (The Serious Stuff)
Okay, so far we’ve covered the basics, but it’s important to know when blood pooling isn’t just a minor inconvenience. If you experience any of the following, seek medical attention immediately:
- Sudden, Severe Leg Pain and Swelling: Especially if accompanied by warmth, redness, or tenderness in the affected area. This could be a sign of a DVT.
- Chest Pain or Shortness of Breath: These symptoms, especially if they occur with leg pain and swelling, could indicate that a blood clot has traveled to your lungs (pulmonary embolism), which is a life-threatening condition.
- Skin Ulcers or Sores: Open sores on your legs, especially around your ankles, can be a sign of severe venous insufficiency and require medical treatment.
- Significant Skin Discoloration: Pronounced bluish or reddish discoloration of your skin, especially if it’s accompanied by pain or swelling, warrants a doctor's visit.
- Blood Pooling Symptoms that Don't Improve with Self-Care: If you've tried the home remedies mentioned above and your symptoms aren't improving, it's time to see a doctor to rule out underlying medical conditions.
- Any New or Worsening Symptoms: If you're concerned about your symptoms, it's always best to err on the side of caution and seek medical advice.
Basically, listen to your body! If something feels seriously wrong, don't wait. Get it checked out.
Final Thoughts (And Leg Love)
Blood pooling in the legs is a common problem, and for many people, it’s just a temporary annoyance. But it’s also a reminder that our bodies are complex systems that need a little TLC. Simple things like elevating your legs, moving around, and wearing compression stockings can go a long way in keeping your circulation healthy.
And remember, if you're ever concerned about your symptoms, don't hesitate to talk to your doctor. They can help you determine the cause of your blood pooling and recommend the best course of treatment.
So, go forth and treat your legs with kindness! They carry you around all day, after all. They deserve it.