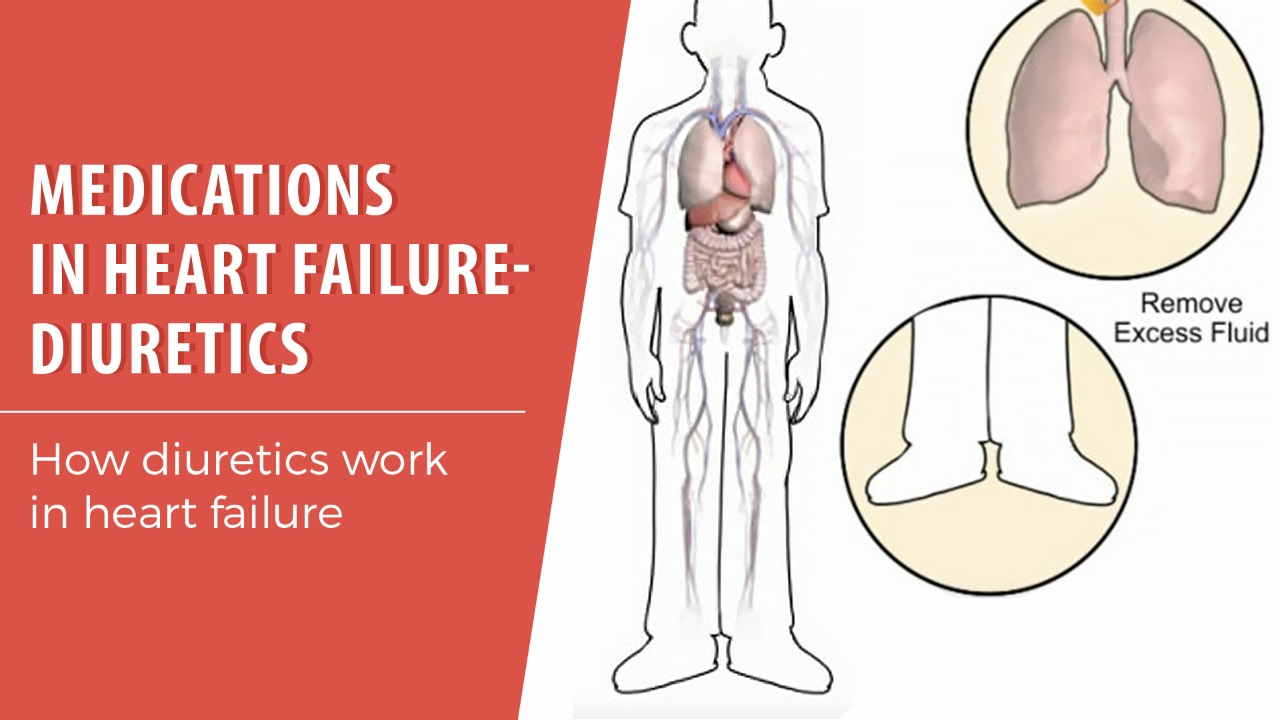
Diuretics, commonly known as water pills, are a cornerstone of heart failure management. They work by helping the kidneys remove excess fluid and sodium from the body, thereby reducing the workload on the heart and alleviating symptoms such as shortness of breath and swelling. However, knowing when to reduce or discontinue diuretic therapy in heart failure is a complex decision, requiring careful consideration of the patient's individual circumstances, clinical status, and overall treatment goals. This article will outline the factors involved in determining when it might be appropriate to stop diuretics in heart failure.
Understanding Diuretics and Heart Failure
Before discussing when to stop diuretics, it's crucial to understand their role in heart failure and the potential consequences of both over- and under-utilization. Heart failure is a chronic condition where the heart is unable to pump enough blood to meet the body's needs. This often leads to fluid retention, causing symptoms like:
- Shortness of breath (dyspnea)
- Swelling in the ankles, legs, and abdomen (edema)
- Fatigue
- Weight gain
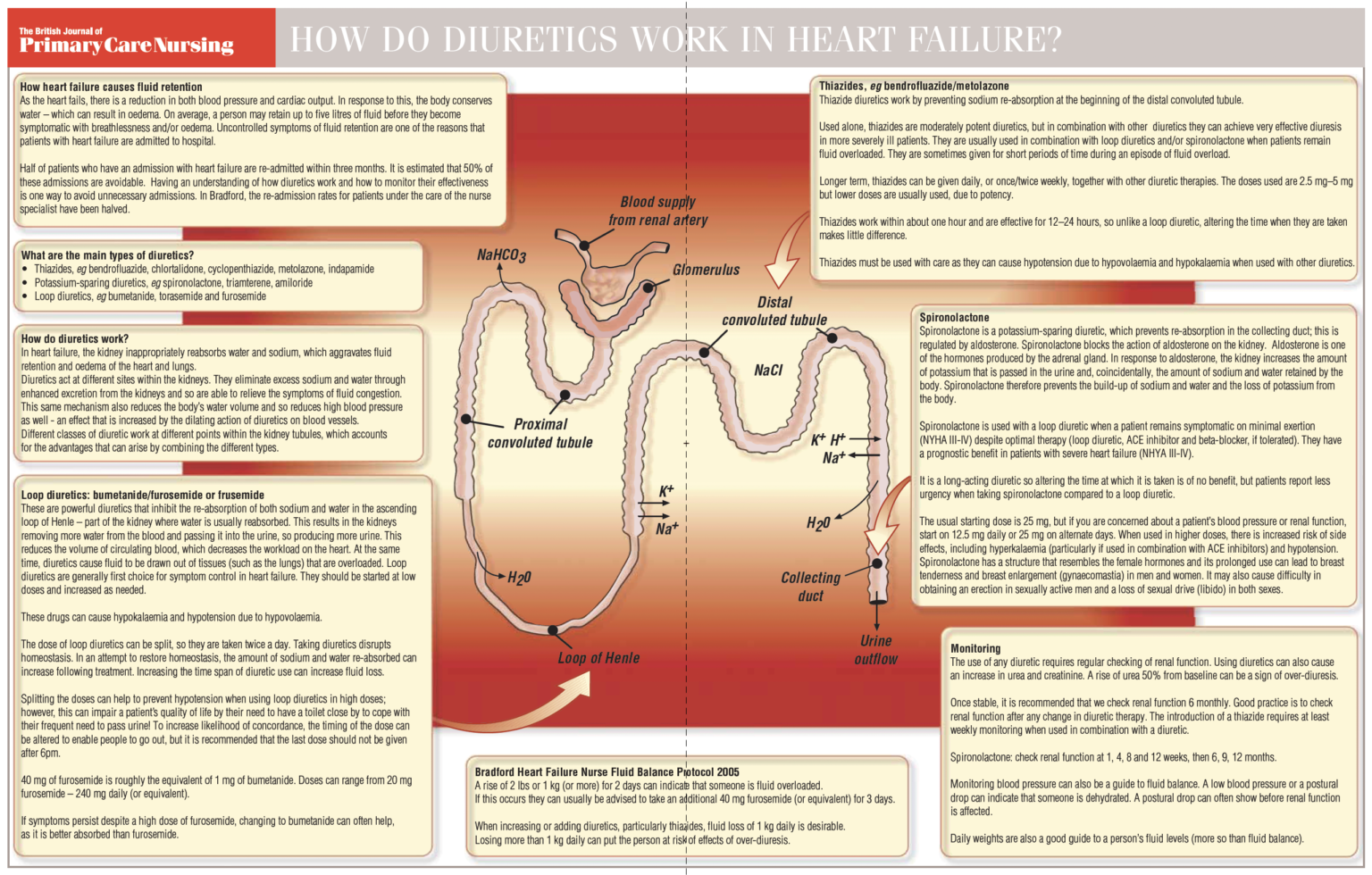
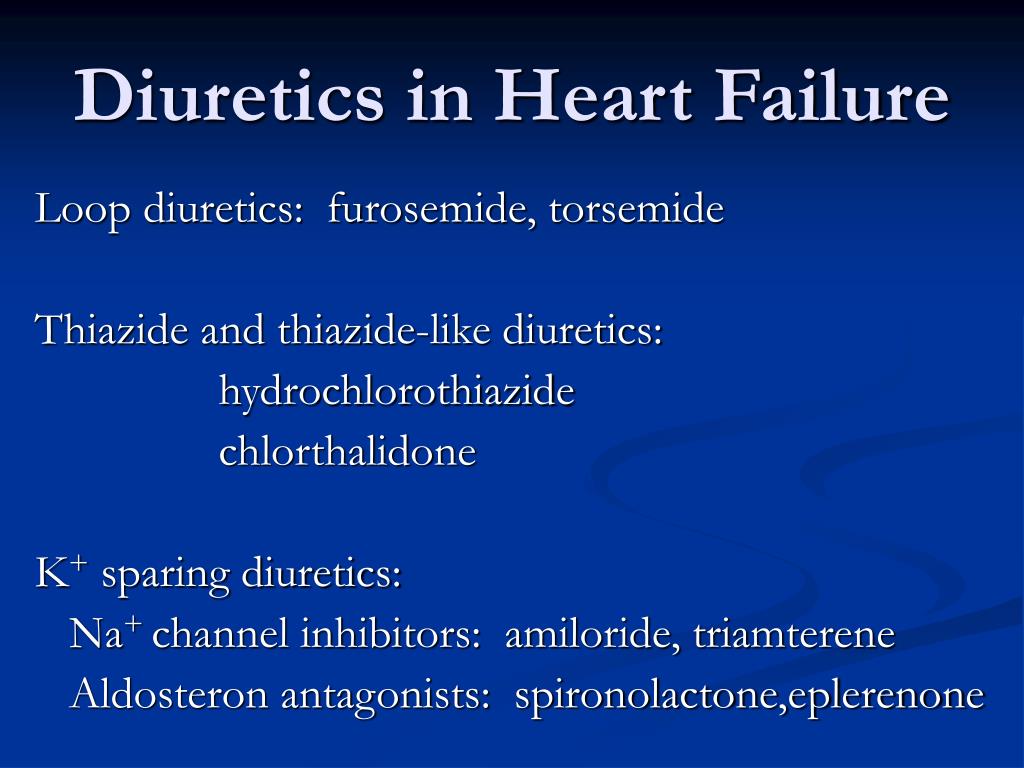
Diuretics help to manage these symptoms by increasing urine production and reducing fluid overload. Common diuretics used in heart failure include:
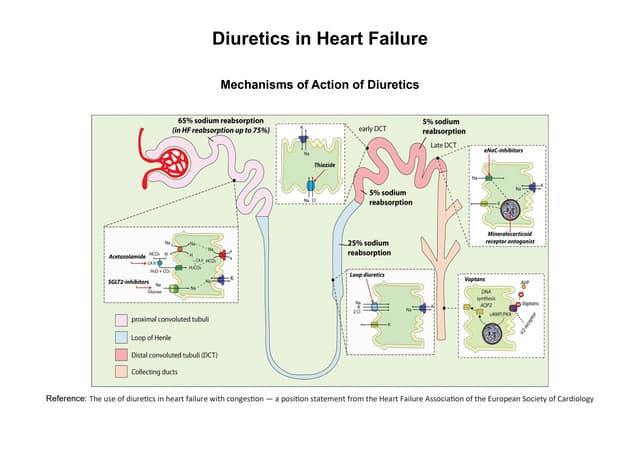
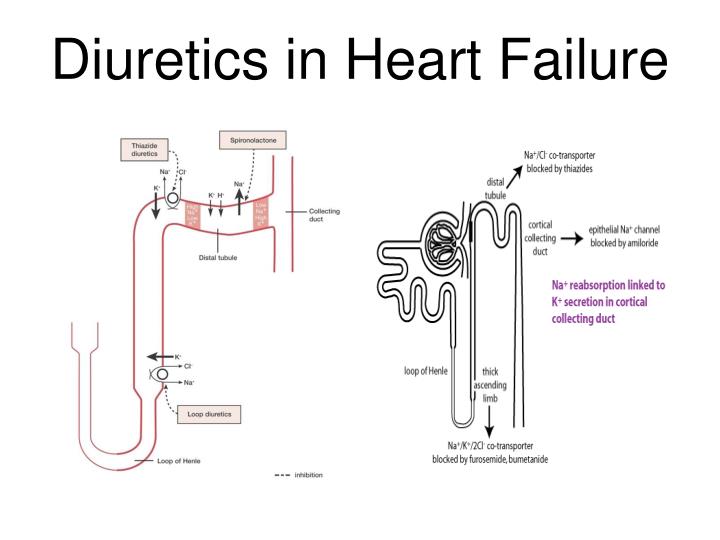
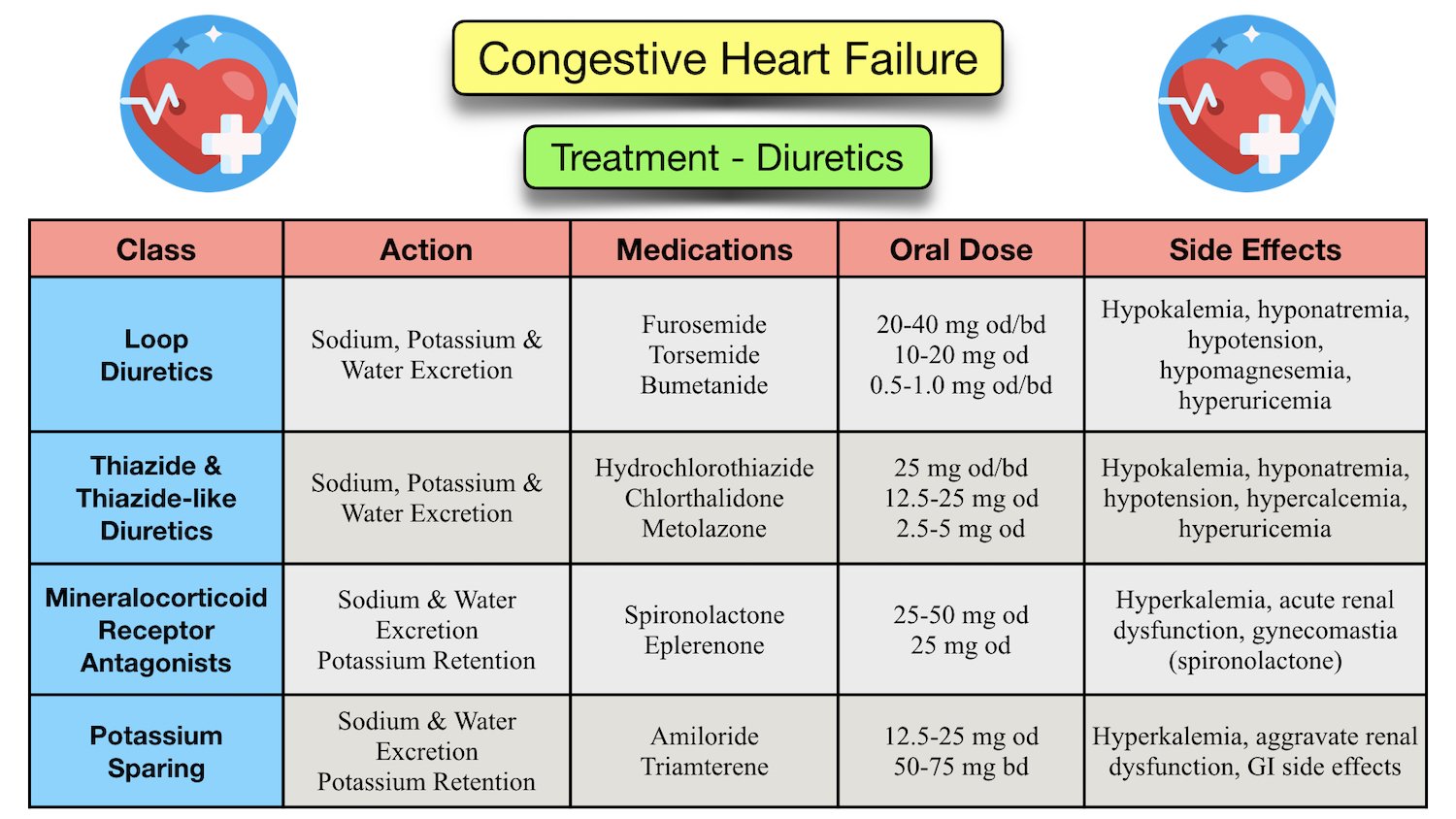
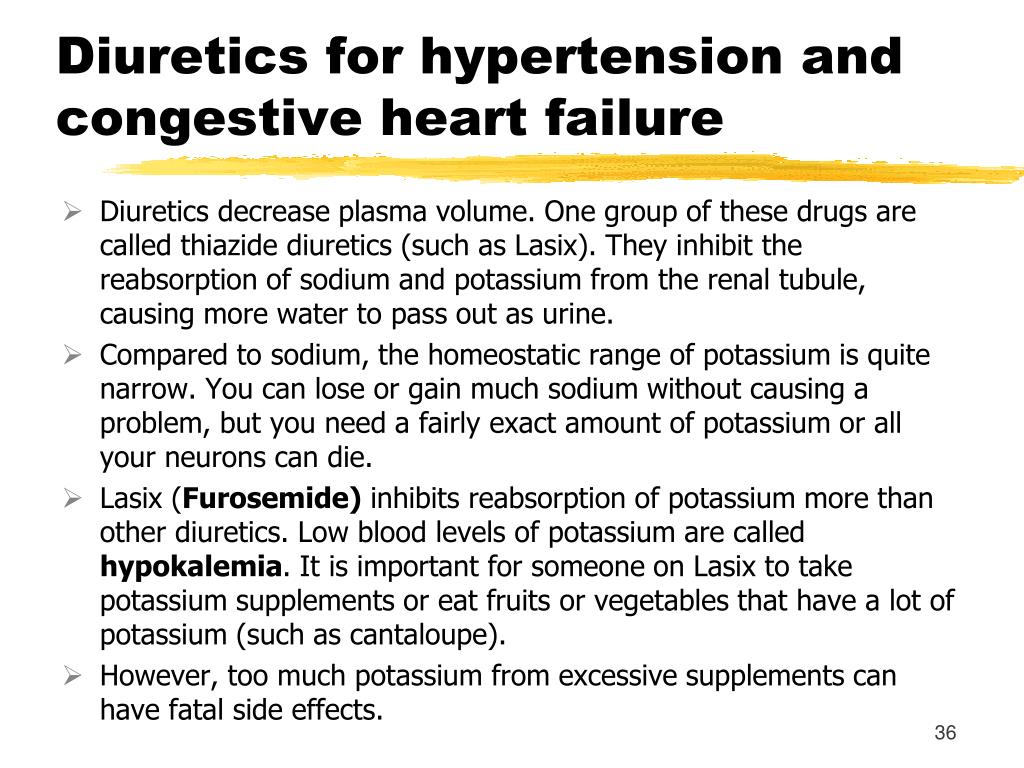
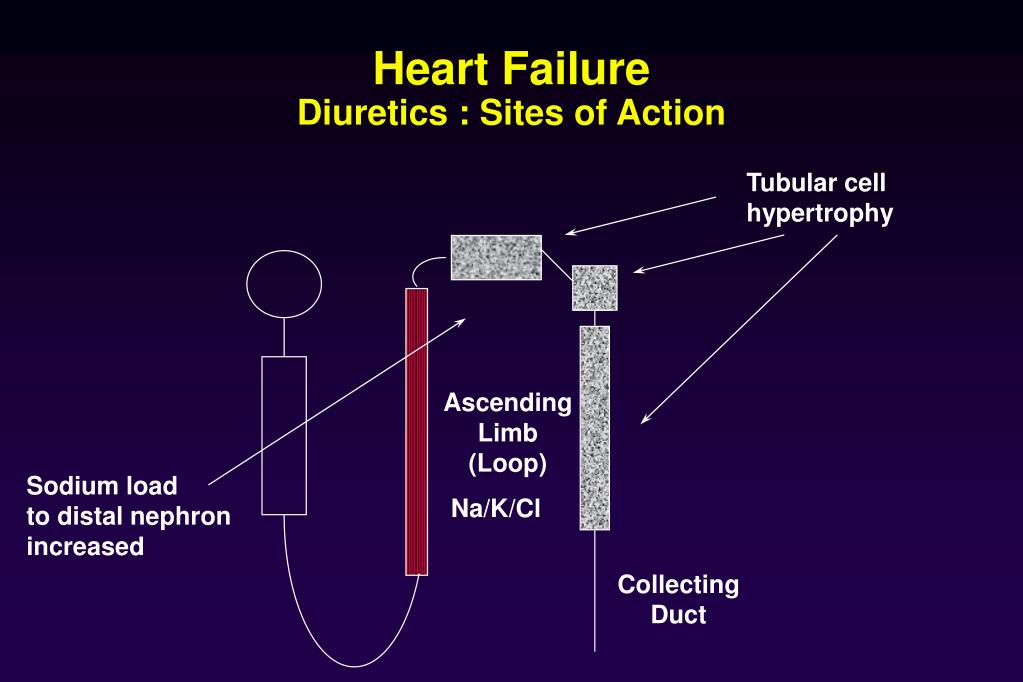
- Loop diuretics: Furosemide (Lasix), bumetanide (Bumex), torsemide (Demadex). These are potent diuretics that work in the loop of Henle in the kidneys.
- Thiazide diuretics: Hydrochlorothiazide (HCTZ), chlorthalidone. These are less potent than loop diuretics and work in the distal convoluted tubule.
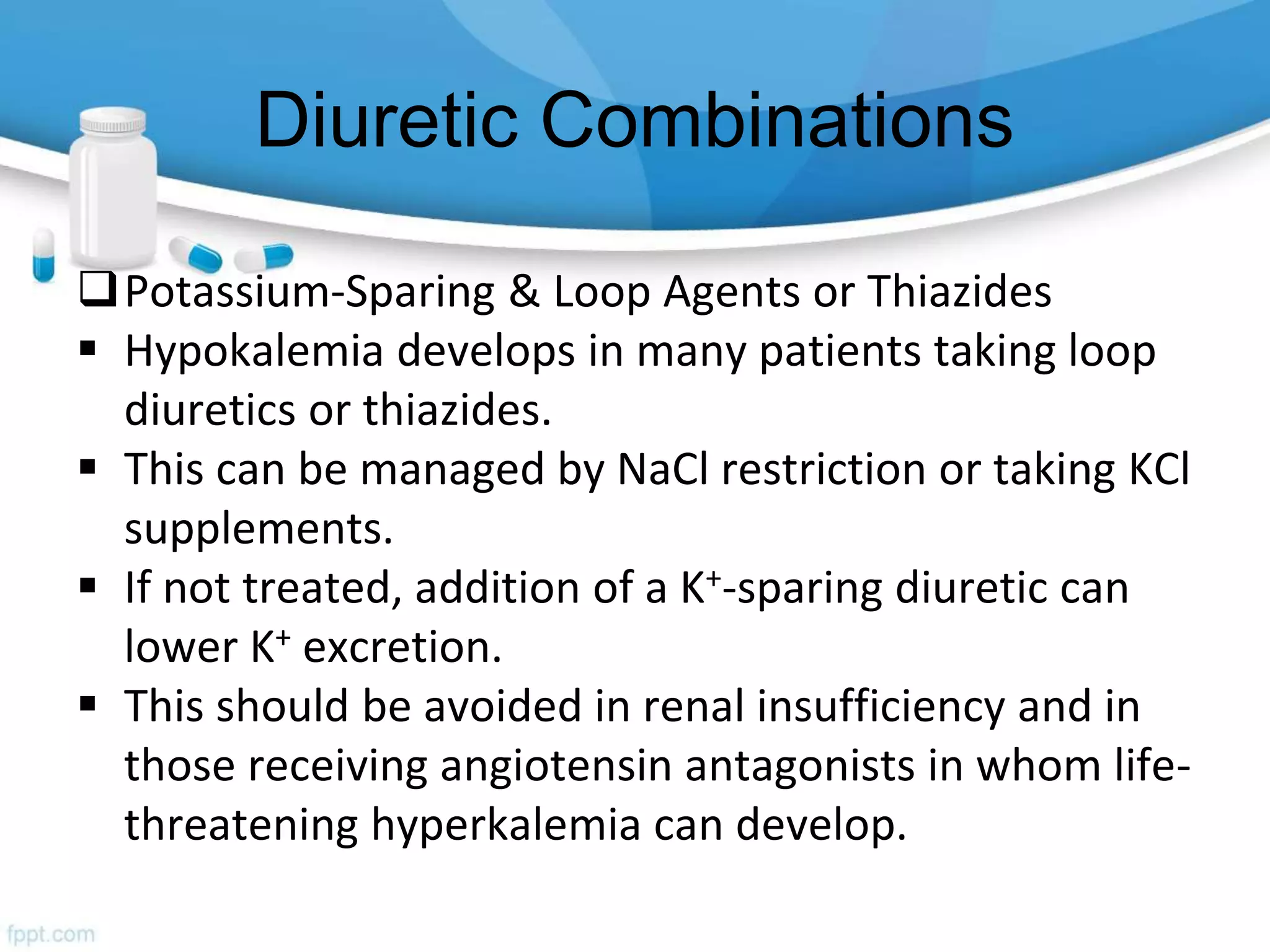
- Potassium-sparing diuretics: Spironolactone (Aldactone), eplerenone (Inspra). These diuretics help to conserve potassium levels in the body.
While diuretics are effective in alleviating symptoms, they don't address the underlying causes of heart failure. Furthermore, inappropriate use can lead to:
- Dehydration: Excessive fluid removal can lead to dehydration, causing dizziness, lightheadedness, and even kidney damage.
- Electrolyte imbalances: Diuretics can deplete essential electrolytes like sodium, potassium, and magnesium, leading to arrhythmias and muscle weakness.
- Kidney dysfunction: Overuse of diuretics can strain the kidneys and worsen kidney function, especially in patients with pre-existing kidney disease.
- Hypotension: Lowering blood volume too much can cause low blood pressure, leading to falls and other complications.
Factors Influencing Diuretic Discontinuation
The decision to stop diuretics in heart failure is not a one-size-fits-all approach. It requires a thorough assessment of several factors, including:
1. Clinical Stability and Symptom Control
The primary consideration is the patient's clinical stability. If the patient has been stable for a prolonged period with minimal or no symptoms of fluid overload, a gradual reduction in diuretic dosage might be considered. "Stable" generally means that the patient has been maintaining their weight, has no significant edema, and experiences no or very little shortness of breath for several weeks or months. A common example would be a patient who has been on a stable dose of furosemide 40mg daily for six months, and during that time, their weight has remained consistent, they have had no hospitalizations for heart failure exacerbation, and they report no significant symptoms of fluid retention.
2. Optimization of Other Heart Failure Therapies
Before considering diuretic discontinuation, it's essential to ensure that all other heart failure medications, such as ACE inhibitors, ARBs, beta-blockers, and mineralocorticoid receptor antagonists (MRAs), are optimized. These medications work synergistically to improve heart function and reduce the need for diuretics. For example, if a patient is not on the maximum tolerated dose of a beta-blocker due to initial side effects but those side effects have subsided, up-titrating the beta-blocker may improve heart function and allow for a reduction in diuretic dosage. Similarly, initiation or optimization of an SGLT2 inhibitor, a newer class of heart failure medication, can have diuretic-sparing effects.
3. Etiology of Heart Failure
The underlying cause of heart failure can influence the decision to stop diuretics. For example, in patients with heart failure due to a reversible cause, such as uncontrolled hypertension or a treatable valve disorder, addressing the underlying cause may lead to improved heart function and reduced need for diuretics. Conversely, in patients with advanced heart failure due to irreversible damage, such as severe cardiomyopathy, diuretics may be necessary for long-term symptom control.
4. Kidney Function
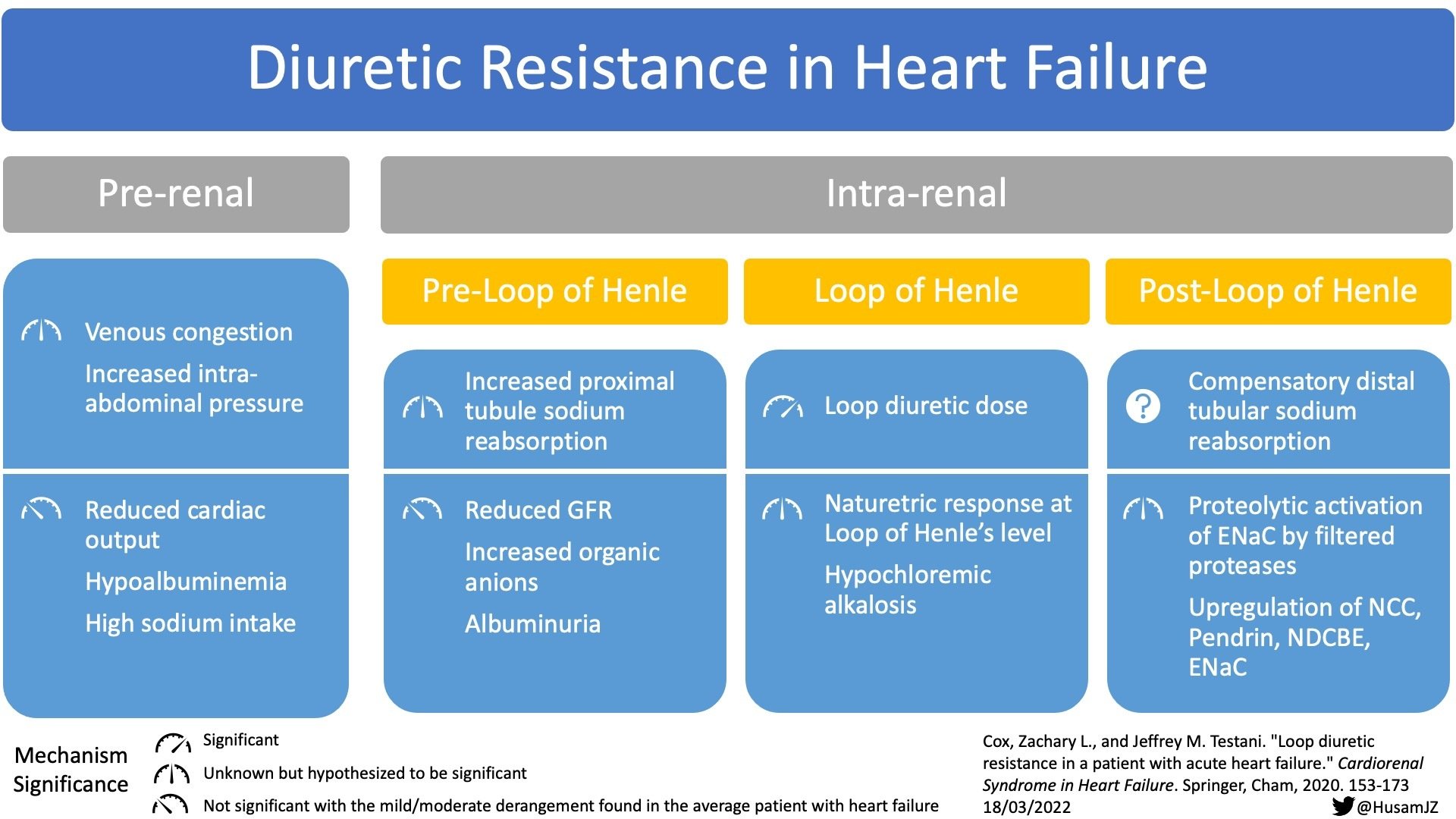
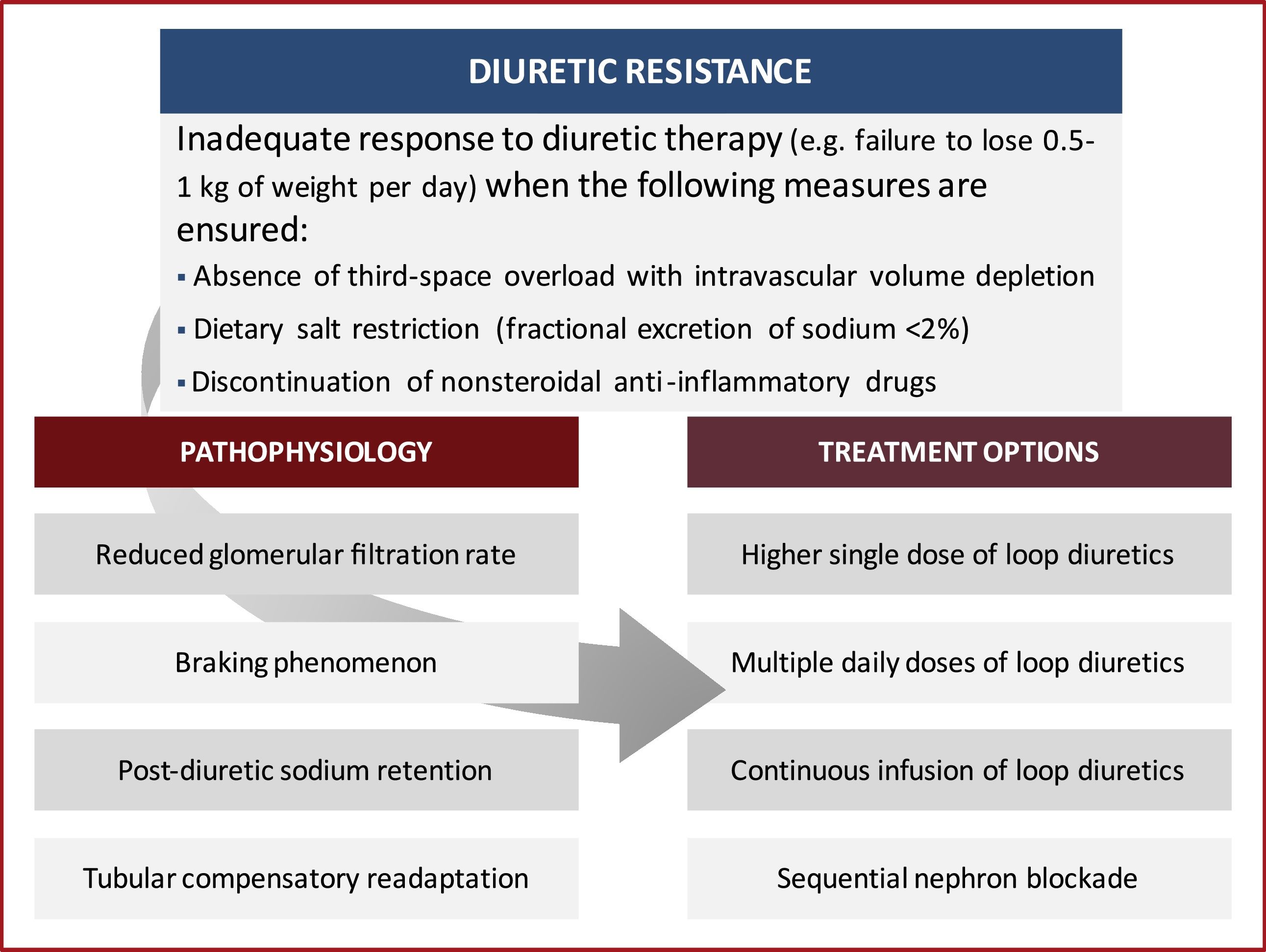
Kidney function is a crucial consideration. Diuretics can affect kidney function, and pre-existing kidney disease can make patients more susceptible to diuretic-related complications. If kidney function deteriorates significantly while on diuretics, a reduction in dosage or a switch to a different type of diuretic may be necessary. Close monitoring of kidney function (e.g., serum creatinine, BUN, eGFR) is essential during diuretic therapy.
5. Electrolyte Levels
Diuretics can cause electrolyte imbalances, such as hypokalemia (low potassium), hyponatremia (low sodium), and hypomagnesemia (low magnesium). These imbalances can lead to arrhythmias, muscle weakness, and other complications. If significant electrolyte abnormalities develop, the diuretic dosage may need to be adjusted or supplemented with electrolyte replacement therapy. Potassium-sparing diuretics may be considered to mitigate potassium loss. Regular monitoring of electrolyte levels is crucial.
6. Patient Preferences and Lifestyle
Patient preferences and lifestyle also play a role in the decision-making process. Some patients may be bothered by the frequent urination associated with diuretic use and may prefer to reduce or discontinue them if possible. However, it's essential to educate patients about the potential risks of stopping diuretics and to involve them in the decision-making process. A patient who travels frequently may find it difficult to manage diuretic therapy and might prefer a strategy that minimizes the need for frequent bathroom breaks.
The Process of Diuretic Discontinuation
If, after considering all the above factors, it is determined that a trial of diuretic reduction is appropriate, it should be done gradually and under close medical supervision. A sudden cessation of diuretics can lead to rapid fluid accumulation and worsening of heart failure symptoms.
- Gradual Reduction: The diuretic dosage should be reduced gradually, typically by 25-50% every few days or weeks, depending on the patient's tolerance. For example, if a patient is taking furosemide 40mg daily, the dosage could be reduced to 20mg daily for a week or two, followed by further reductions as tolerated.
- Close Monitoring: During the diuretic reduction period, patients should be closely monitored for signs of fluid overload, such as weight gain, edema, and shortness of breath. Daily weight monitoring is crucial. Patients should be instructed to contact their healthcare provider immediately if they experience any worsening symptoms.
- Adjustment Based on Response: If the patient develops signs of fluid overload, the diuretic dosage should be increased back to the previous effective dose. If the patient remains stable, further reductions can be considered. In some cases, it may be possible to discontinue diuretics altogether, while in others, a low maintenance dose may be necessary to maintain stability.
- Patient Education: Patient education is paramount. Patients need to understand the importance of adhering to dietary sodium restrictions, monitoring their weight, and recognizing the signs and symptoms of fluid overload. They should also be educated on how to adjust their diuretic dosage based on their symptoms, under the guidance of their healthcare provider.
Practical Advice and Insights
While this article provides a comprehensive overview of when to stop diuretics in heart failure, it's important to remember that each patient is unique, and the decision-making process should be individualized. Here are some practical insights for everyday life:
- Work closely with your healthcare provider: Don't attempt to adjust your diuretic dosage on your own. Always consult with your doctor or other qualified healthcare professional before making any changes to your medication regimen.
- Monitor your weight daily: Weight gain is often the earliest sign of fluid overload. By monitoring your weight daily, you can detect fluid accumulation early and take appropriate action.
- Adhere to dietary sodium restrictions: Reducing your sodium intake can help to reduce fluid retention and the need for diuretics. Aim for a sodium intake of less than 2000mg per day.
- Be aware of the signs and symptoms of fluid overload: Know the signs and symptoms of fluid overload, such as shortness of breath, edema, and weight gain, and report any worsening symptoms to your healthcare provider promptly.
- Keep a medication list: Maintain an accurate and up-to-date list of all your medications, including diuretics, and share it with your healthcare providers.
Ultimately, the goal of heart failure management is to improve quality of life and reduce the risk of hospitalization and death. While diuretics play a crucial role in symptom control, it's important to use them judiciously and to consider the potential risks and benefits of diuretic therapy in the context of the patient's overall clinical picture.